Keratitis: causes, symptoms, and treatment methods
- Definition of keratitis
- Factors contributing to the development of keratitis
- Manifestations of keratitis
- Approaches to the treatment of keratitis
- Methods for diagnosing keratitis
- Methods of treating keratitis
- Measures for the prevention of keratitis
- It is necessary to study experts’ views on possible methods of preventing keratitis in light of medical research.
- FAQ
Definition of keratitis
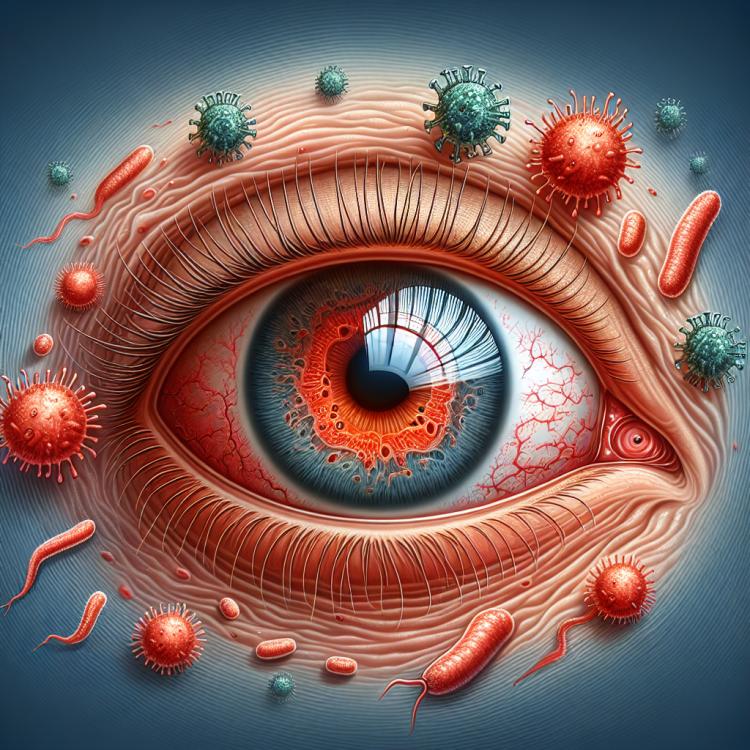
Keratitis is an inflammatory disease of the cornea of the eye, characterized by impairment of its transparency and function. This condition is usually caused by infection, trauma, or immune reactions. Patients with keratitis often experience pain, redness of the eye, a sensation of a foreign body, and blurred vision, which requires timely diagnosis and appropriate treatment to prevent the development of complications.
Factors contributing to the development of keratitis
Keratitis can be caused by various factors, including microorganisms, eye trauma, chemical exposures, or autoimmune reactions. Infectious agents such as bacteria, viruses, fungi, or parasites can penetrate the cornea through damaged surfaces or contact lenses, causing inflammation. Eye trauma, including scratches, burns, or surgical intervention, can also be a cause of keratitis by creating an entry point for infection or irritation of the eye tissues.
- Microorganisms: Bacteria, viruses, fungi, or parasites can penetrate the cornea through a damaged surface or contact lenses, contributing to the development of keratitis.
- Eye injury: Scratches, burns, surgical interventions, or other damage to the eye can create access for infection or irritation, provoking an inflammatory response.
- Chemical exposure: Exposure to aggressive chemicals can damage the cornea and promote the development of keratitis.
- Autoimmune reactions: Some autoimmune diseases can lead to inflammatory processes in the eyes, which may be associated with the development of keratitis.
- Wearing contact lenses: Improper use or careless handling of contact lenses can increase the risk of developing infectious keratitis.
Manifestations of keratitis
Keratitis is characterized by various symptoms, including eye pain, a sensation of a foreign body, photophobia, tearing, blurred vision, and redness of the eye. Patients may experience a decrease in visual clarity due to disruption of the smoothness of the corneal surface, leading to various anomalies in the perception of the surrounding world. Diagnosis and treatment of keratitis require careful examination of symptoms and appropriate clinical studies for accurate diagnosis and optimal therapy.
- Pain in the eye: patients may feel discomfort and painful sensations, especially when blinking or moving their eyes.
- Foreign body sensation: patients may feel that there is a foreign object in their eye, even if its absence is confirmed by a visual inspection.
- Photophobia: patients experience increased sensitivity to bright light, which can cause discomfort and worsening of vision.
- Tearing: keratitis can cause increased tearing, which may be a natural reaction to irritation or the result of infection or inflammation.
- Blurriness of vision: due to changes in the structure and function of the cornea, patients may experience a disturbance in visual clarity and see images indistinctly and blurred.
Approaches to the treatment of keratitis
Experts in the field of ophthalmology recommend an individualized approach to the treatment of keratitis depending on the type and severity of the disease. Treatment may include the use of antibiotics, antiviral agents, antifungal medications, or steroids, depending on the causative agent and the stage of the inflammatory process. However, the prescription of treatment should be conducted under the supervision of a specialist to avoid complications and ensure the optimal regimen for taking medications.
Experts also emphasize the importance of regular medical monitoring and control of the condition of the corneal surface during the treatment of keratitis. If necessary, surgical intervention may be required to restore the integrity of the cornea and prevent further complications. Adhering to specialists’ recommendations and seeking assistance in a timely manner contribute to successful treatment and recovery of eye health.

Methods for diagnosing keratitis
The diagnosis of keratitis is based on a visual examination of the eye using tools such as a slit lamp, which allows the doctor to examine the cornea and assess its condition. In addition, additional studies may be conducted, such as analysis of the discharge from the eye, biomicroscopy, visual acuity measurement, and intraocular pressure assessment. These methods allow for the diagnosis of the type of keratitis, determination of its severity, and identification of possible complications, which aids in the effective prescription of treatment and monitoring of the outcome.
- Visual inspection: using a slit lamp for detailed examination of the cornea and evaluation of its condition.
- Analysis of eye discharge: conducting laboratory studies of smears to identify possible microorganisms causing keratitis.
- Biomicroscopy: a method of examining the eye fundus for detailed study of changes on the surface of the cornea.
- Determination of visual acuity: assessing the degree of reduction in visual function to evaluate the impact of keratitis on visual abilities.
- Methods for measuring intraocular pressure: analysis of pressure readings in the eye can be important in diagnosing keratitis and assessing its impact on eye health.
Methods of treating keratitis
- Use of antibiotics: antibiotics can be used to combat bacterial infection, which is one of the common causes of keratitis.
- Use of antifungal medications: when a fungal infection of keratitis is identified, it may be necessary to use antifungal agents for effective treatment.
- Use of steroid drops: steroid medications may be used to reduce inflammation and prevent complications in certain types of keratitis.
- Use of antiviral medications: in cases where keratitis is caused by a viral infection, the use of antiviral medications may be required for effective treatment and infection control.
- Individual approach to treatment: each case of keratitis is unique, so it is important to conduct a detailed diagnosis and assess the risks and benefits of various treatment methods to determine the optimal therapeutic approach.
Measures for the prevention of keratitis
- Compliance with hygiene rules when using contact lenses: includes regular cleaning and disinfection of lenses, as well as adhering to replacement schedules.
- Use of personal protective equipment: when working in conditions of increased dust or chemicals, one should protect the eyes to prevent possible irritation and injuries.
- Avoiding contact with potential sources of eye injury: reduces the likelihood of injuries that may contribute to the development of keratitis.
- Timely consultation with a doctor at the first signs of eye inflammation: will help diagnose and treat any infections or inflammations of the eye promptly to prevent the occurrence of keratitis.
- Regular preventive examinations by an ophthalmologist: will help identify any initial changes in the condition of the eyes and take measures to prevent or initiate early treatment.