Keratosis: symptoms, causes, and treatment
Understanding Keratoma: Key Facts
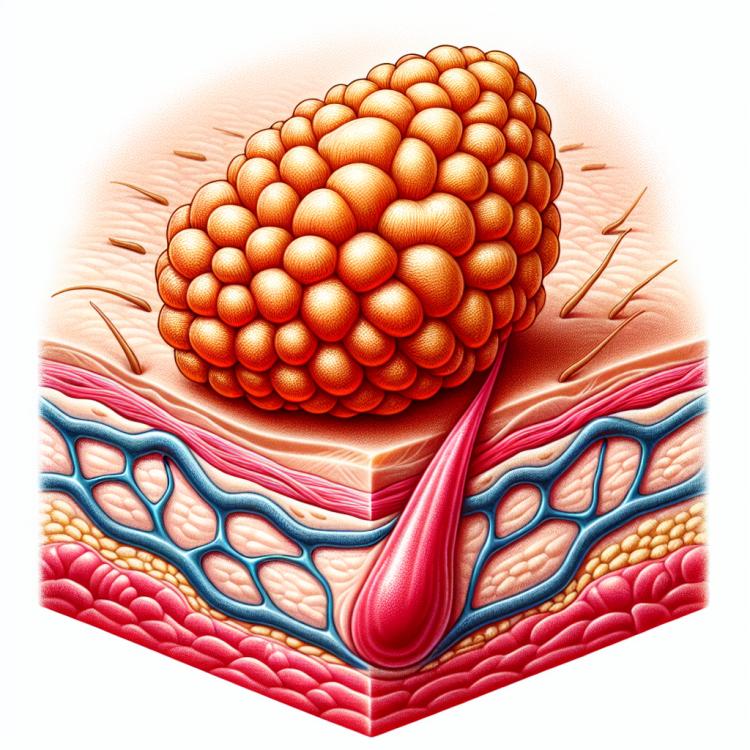
Keratosis is a benign tumor that arises from the cells of the epidermis. This condition often manifests as dense, raised formations on the skin, frequently ranging in color from beige to brown. The causes of keratoses can be diverse, including genetic factors, frequent exposure to ultraviolet radiation, and age-related skin changes.
Management of keratoses may include conservative treatments such as cryotherapy or laser removal, especially if the tumor causes discomfort or cosmetic issues. Since keratoses are generally benign, the prognosis is usually favorable after effective treatment and monitoring.
Pathogenesis of keratoma
Keratoma is a benign neoplasm caused by hyperplasia of the epidermis or skin appendages, leading to excessive keratin formation in the surface layers of the skin. The main causes of keratoma development include chronic skin trauma, sun exposure, genetic predisposition, and age-related changes. Chronic mechanical action on the skin can lead to local hyperplasia of the epidermis and the formation of keratoma, while sun exposure contributes to the accumulation of mutations in the skin, promotes the activation of oncogenes, and the development of neoplasms. Genetic factors may also play a role in the occurrence of keratoma, especially in individuals with a family history of certain skin diseases.
- Hyperplasia of the epidermis: Keratoma is characterized by excessive growth of the epidermis or skin appendages, leading to the formation of hyperkeratosis.
- Mechanical damage: Chronic skin trauma, such as from friction or pressure, can contribute to the development of keratoma.
- Solar radiation: Ultraviolet rays can damage the DNA of skin cells, activating mutagenesis and carcinogenesis processes.
- Genetic predisposition: Hereditary factors may increase the likelihood of developing keratoma in some individuals.
- Age-related changes: With age, the skin ages, undergoes photoaging, which in turn can contribute to the development of keratoma.
The clinical picture of keratoma
The clinical picture of a keratosis may include the appearance of single or multiple nodules of various colors ranging from yellowish to brown on the skin. These nodules typically range in size from a few millimeters to several centimeters and have clear borders. The surface of the keratoses can be smooth or rough, sometimes covered with a crust, indicating possible traumatic impact on the formation. Usually, keratoses do not cause pain, but discomfort and itching may arise when they reach larger sizes or become damaged.
For a comprehensive assessment of the clinical picture of keratosis, it is important to consider the localization of the formation, its shape, size, color, texture, and changes in the surrounding tissue. Given the possible similarity to other skin neoplasms, such as basal cell carcinoma, differential diagnosis must be performed based on indirect signs, pathological analysis, medical history, and other supplementary studies.
- Appearance of nodules: keratomas may appear as single or multiple nodules of various shades, with clear borders.
- Size and shape of formations: the size of keratomas can range from a few millimeters to several centimeters, and the shape can be round, oval, or irregular.
- Surface of the keratoma: the surface of the formation can be smooth or rough, sometimes with a crust or horn-like scales.
- Color shades: keratomas can have different colors, including yellowish, brown, or black, depending on the type and stage of development.
- Accompanying symptoms: keratomas usually do not cause pain, but when traumatized or irritated, they may be accompanied by itching, discomfort, or bleeding.
Experts’ views on keratoma therapy
The expert opinion on the treatment of keratoma is based on a comprehensive approach to managing this condition. Depending on the size, location, characteristics of the lesion, and the patient’s preferences, various therapeutic methods may be suggested. Surgical removal of the keratoma may be necessary in cases of large tumor size, rapid growth, changes in color or texture, or when symptoms of discomfort occur.
Experts also emphasize the importance of prevention and regular monitoring of keratomas to prevent possible complications and recurrences. It is best to consult a qualified dermatologist or oncodermatologist to obtain personalized treatment, skincare recommendations, and to maintain regular surveillance of the keratomas and overall skin health.

Methods of diagnosing keratoma
Diagnosis of keratoma usually begins with a visual inspection and assessment of the clinical signs of the skin neoplasm. To confirm the diagnosis and exclude other possible skin pathologies, dermatoscopy may be recommended – a method of viewing skin formations under magnification using a dermatoscope. If necessary, a biopsy may be prescribed, where a section of skin with the keratoma is extracted for pathological histological analysis to identify structural features and determine the nature of the neoplasm.
Additional diagnostic methods, such as skin ultrasound, computed tomography (CT), or magnetic resonance imaging (MRI), may be used in cases where there is suspicion of the spread of the neoplasm into deeper tissues or organs. Careful diagnosis of keratoma allows for determining the optimal treatment approach and ensuring the best outcomes for the patient.
- Visual inspection: initial assessment of the clinical signs of keratoma is conducted by a specialist during the patient’s visit.
- Dermatoscopy: a method of careful examination of skin lesions under magnification using a dermatoscope for a more detailed assessment of the structure and color of the keratoma nodules.
- Biopsy: a procedure in which a small area of skin with a keratoma is removed for subsequent pathologic and histological analysis for an accurate diagnosis.
- Ultrasound examination: may be used to assess the depth of skin infiltration and determine the structural characteristics of the neoplasm.
- Computed tomography (CT) and magnetic resonance imaging (MRI): in cases of suspected invasion of the keratoma into deeper tissues, these studies may be prescribed for further evaluation.
Methods of treating keratoma
After the removal of the keratoma, it is important to follow the doctor’s recommendations for skin care and preventing recurrences. Regular monitoring and screening for other skin changes may also be necessary to maintain overall skin health. It is important to consult a dermatologist or oncologist to choose the most appropriate treatment method for keratoma in each individual case.
- Surgical removal: one of the treatment methods for keratosis is its removal through surgical intervention, such as excision or destruction by special techniques like cryotherapy, electrosurgery, or laser. These procedures help effectively eliminate keratosis and prevent its recurrence.
- Nimesulide (a drug with anti-inflammatory action): some studies have shown the effectiveness of treating keratosis using the topical application of nimesulide.
- Cryotherapy: a treatment method in which keratosis is removed by freezing the tissues using liquid nitrogen or another cryogen, leading to their destruction.
- Electrosurgery: an effective treatment method in which keratosis is removed using electric current, allowing for quick and precise removal of the affected skin area.
- Laser therapy: the use of laser radiation to remove keratosis with precise effects on the affected tissue, ensuring minimal risk of damage to surrounding tissues and good cosmetic efficacy.
Preventive measures for keratoma
- Use of sunscreen: Regular application of SPF products helps protect the skin from harmful ultraviolet radiation, which can contribute to the development of keratosis.
- Wearing protective clothing and hats: Clothing with protective properties helps prevent direct exposure of ultraviolet rays to the skin, reducing the risk of keratosis.
- Regular skin check-ups with a dermatologist: Conducting preventive skin examinations allows for the early detection of changes and neoplasms, helping to prevent the development of keratosis.
- Avoiding excessive mechanical impact on the skin: Preventing injuries and mechanical impacts on the skin helps reduce the likelihood of keratosis formation due to chronic trauma.
- Systematic monitoring and self-examination for changes in the skin: Pay attention to any new or increasing formations, moles, or pigmented spots on the skin and seek medical advice immediately if they appear.