Cholangitis: symptoms, causes, and treatment
Description of Cholangitis
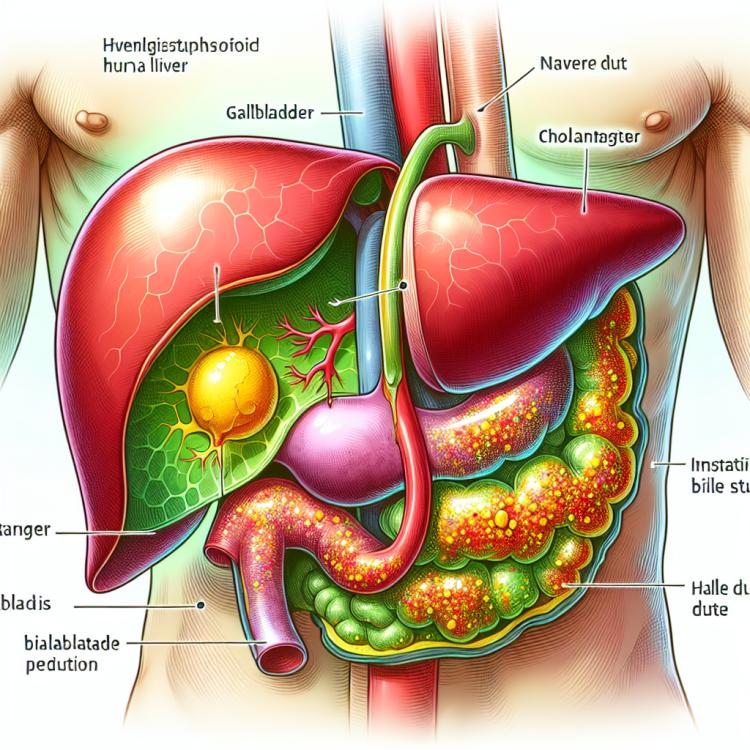
Cholangitis is an inflammatory disease of the bile ducts, usually caused by an infection. The pathogenesis of this disease is most often associated with the penetration of bacteria into the biliary tract, leading to their inflammation. Cholangitis can present with various symptoms, including jaundice, pain in the right upper quadrant, fever, nausea, and vomiting. Various methods may be used for the diagnosis of cholangitis, such as ultrasound examination, computed tomography, biochemical blood tests, endoscopy, and others.
The treatment of cholangitis depends on its form and severity. Antibiotics are usually used to combat the infection, as well as procedures to remove formed stones or obstructions in the bile ducts. In some cases, surgical intervention may be required. Early detection and timely treatment of cholangitis are crucial for preventing complications and restoring normal functioning of the biliary system.
Etiology of Cholangitis
Cholangitis, an inflammatory disease of the bile duct, can be caused by various factors. One of the primary causes is bile stagnation in the bile duct, which can promote the multiplication of bacteria and the development of infection. Another common cause of cholangitis is mechanical problems, such as gallstones or tumors, which can hinder the normal flow of bile and contribute to the development of inflammation.
- Bile stasis: Disorders in bile flow can contribute to the proliferation of bacteria and the development of inflammation.
- Bile stones: The formation of stones in the gallbladder or ducts can cause a mechanical obstruction and promote the development of cholangitis.
- Gallbladder tumors: The presence of tumors in the bile ducts can lead to their compression and inflammation.
- Infectious agents: Bacteria or viruses entering the bile ducts can cause infection and cholangitis.
- Autoimmune disorders: In some cases, cholangitis may be triggered by the body’s autoimmune reaction to its own bile ducts.
Clinical picture of Cholangitis
Cholangitis is characterized by a variety of clinical manifestations. Patients often complain of pain in the right upper quadrant, which can be sharp and worsen after consuming fatty foods. In addition, common symptoms of cholangitis also include jaundice, skin itching, general weakness, and elevated levels of bilirubin and alkaline phosphatase in the blood.
In cholangitis, the development of acute cholelithiasis, the occurrence of obstructive syndrome of the gallbladder, the development of liver abscess, or pancreatitis is possible. Defining the clinical picture of cholangitis is crucial for diagnosis and the appropriate treatment plan.
- Pain in the right hypochondrium: patients often experience sharp pain in the right hypochondrium, especially after consuming fatty foods.
- Jaundice: a symptom of cholangitis manifested as a yellow tint of the skin and sclera, associated with impaired bile excretion.
- Itching of the skin: a frequent symptom of cholangitis caused by the accumulation of bile acids in the blood and tissues.
- General weakness: patients with cholangitis often complain of general weakness and deterioration of well-being.
- Elevated levels of bilirubin and alkaline phosphatase in the blood: laboratory indicators characteristic of cholangitis include elevated levels of these substances in the blood.
Expert opinions on the treatment of Cholangitis
Experts in the field of gastroenterology emphasize the importance of a comprehensive approach to the treatment of cholangitis. Depending on the form of the disease and its severity, various therapeutic methods are employed, including conservative treatment, endoscopic drainage of the biliary tract, cholecystectomy, and sometimes even surgical intervention.
Experts note that timely diagnosis and the appointment of appropriate treatment play a crucial role in the prognosis and outcome of the disease. They recommend careful monitoring of the clinical picture, the use of adequate diagnostic methods, and the establishment of an individual treatment scheme in each specific case of cholangitis.

Diagnosis of Cholangitis
Diagnosis of cholangitis is a comprehensive process that includes various examination methods. Initially, the doctor performs a physical examination of the patient and asks about characteristic symptoms. To clarify the diagnosis, blood tests such as a complete blood count, biochemical analysis, and tests for bilirubin levels and liver enzymes may be ordered.
Additional diagnostic methods for cholangitis include ultrasound of the bile ducts, computed tomography (CT) of the abdominal cavity, magnetic resonance cholangiography (MRCP), endoscopic retrograde cholangiopancreatography (ERCP), and other instrumental methods that help doctors accurately establish a diagnosis and determine the optimal treatment for the patient.
- Physical examination: the doctor examines the patient and discusses the characteristic symptoms of cholangitis.
- Laboratory blood tests: a complete blood count, biochemical analysis, bilirubin test, and liver enzyme tests help identify pathological changes.
- Ultrasound examination of the bile ducts: allows visualization of possible changes in the structure of the bile ducts.
- Computed tomography (CT): provides a more detailed image of the abdominal cavity to identify pathologies.
- Magnetic resonance cholangiography (MRCP): a method of detailed examination of the bile ducts using magnetic resonance for the diagnosis of cholangitis.
Treatment of Cholangitis
For the treatment of chronic cholangitis, various methods are used, including drug therapy to control inflammation, as well as dietary regimen and special lifestyle recommendations. In some cases, long-term treatment and regular monitoring by a physician may be required to prevent relapses and maintain the function of the bile ducts.
- Endoscopic dilation of the bile ducts: This method allows for the removal of bile stones and restoration of normal bile flow.
- Antibiotic therapy: The use of antibiotics can help in the fight against the infection that caused cholangitis.
- Use of anti-inflammatory medications: Drugs in this group can help reduce inflammation in the bile ducts.
- Cholecystectomy: In the presence of bile stones, surgical removal of the gallbladder may be recommended to prevent exacerbations of cholangitis.
- Regular monitoring and consultations with a doctor: Patients with chronic cholangitis are advised to have continuous medical monitoring to control their condition and prevent complications.
Prevention of cholangitis
To prevent cholangitis, it is essential to avoid the consumption of alcohol and nicotine, which can negatively impact bile metabolism. Regular physical activity and maintaining a healthy lifestyle also contribute to strengthening the immune system and the overall condition of the body, which is important for the prevention of cholangitis.
- Proper nutrition: Avoid excessive consumption of fatty and spicy foods, which can irritate the bile ducts.
- Fiber-rich diet: Eating foods that contain fiber can promote the health of the bile ducts and prevent cholangitis.
- Quitting harmful habits: Avoid consuming alcohol and cigarettes, as they can negatively affect bile metabolism.
- Physical activity: Regular sports activities contribute to strengthening the immune system and overall health, helping to prevent cholangitis.
- Maintaining a healthy lifestyle: Maintain a healthy psycho-emotional state, monitor your weight, and undergo regular medical check-ups for timely detection of potential problems.
Interesting aspects of Cholangitis
Interestingly, autoimmune disorders can also be among the causes of cholangitis, where the immune system attacks its own liver and bile duct tissues. This aspect demonstrates the importance of further research and the development of new diagnostic and treatment methods for more effective management of cholangitis.