Choledocholithiasis: diagnosis, complications, and prevention
- Understanding Choledocholithiasis
- Factors contributing to the development of choledocholithiasis
- Manifestations of Choledocholithiasis
- The perspective of medical professionals on the treatment of choledocholithiasis.
- Methods for diagnosing choledocholithiasis
- Cholodocholithiasis Therapy
- Preventive measures for choledocholithiasis
- Amazing Aspects of Choledocholithiasis
- FAQ
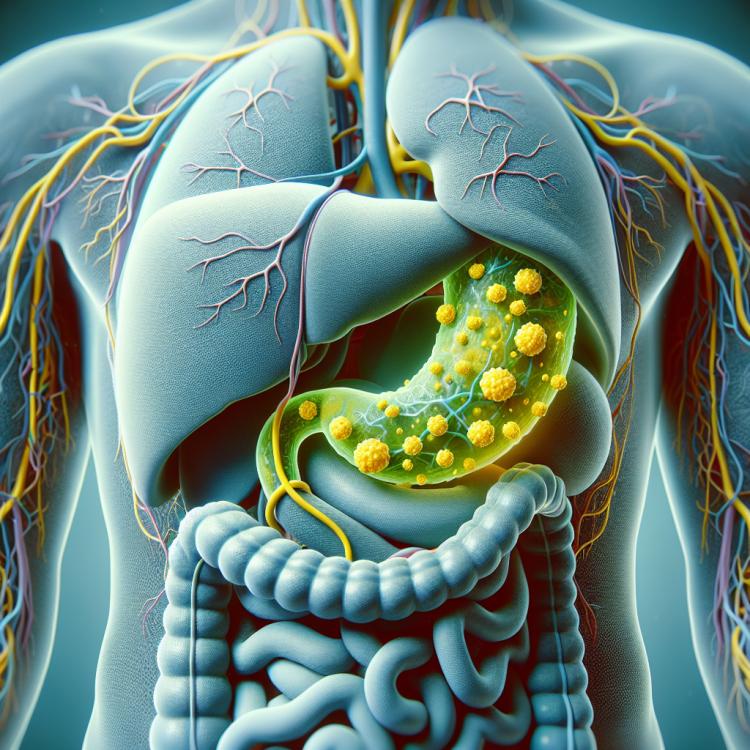
Understanding Choledocholithiasis
Cholelithiasis involves the formation of stones in the common bile duct. This pathological process is most often caused by the migration of stones from the gallbladder. Bile stones can block the bile ducts, causing obstruction and discomfort. The diagnosis of cholelithiasis includes clinical manifestations, laboratory tests, and instrumental methods of examination, such as ultrasound of the gallbladder and bile ducts, CT, or MRCP. Treatment directly depends on the characteristics of cholelithiasis but includes conservative methods, endoscopic retrograde cholangiopancreatography (ERCP), and surgical intervention.
Factors contributing to the development of choledocholithiasis
The development of choledocholithiasis can be caused by several factors. One of them is the impairment of gallbladder function, which leads to the formation of stones in the bile ducts. An elevated level of cholesterol or bilirubin in the bile can also contribute to the formation of stones, causing their deposition in the bile ducts.
The main causes of the development of choledocholithiasis include genetic predisposition, as well as disorders in the bile excretion system, for example, bile secretion and the movement of bile fistulas. The formation of stones can also be due to prolonged use of certain medications, as well as poor diet and metabolic disorders.
- Genetic predisposition: Hereditary factors may contribute to the formation of stones in the bile ducts.
- High cholesterol levels: Increased cholesterol levels in bile can contribute to the formation of stones and their deposition in the bile ducts.
- Unbalanced diet: Regular consumption of fatty, fried foods and products rich in cholesterol may increase the risk of developing choledocholithiasis.
- Long-term use of certain medications: Some drugs may aid in the formation of stones in the bile ducts.
- Disruptions in the bile excretion system: Failures in the secretion of bile acids, bile secretion, and movement of bile fistulas may contribute to the formation of stones.
Manifestations of Choledocholithiasis
Choledocholithiasis, characterized by the presence of stones in the common bile duct, has its distinctive clinical appearance. Patients often complain of pain in the right upper quadrant of the abdomen, which may occur after eating and is accompanied by nausea and vomiting. Worsening of pain during movement or against the background of breathing is a characteristic feature.
In addition, jaundice accompanying cholelithiasis is caused by bile stagnation and can manifest as a yellowing of the skin, mucous membranes, and the sclera of the eyes. Other symptoms may include itching of the skin, dark urine, and pale or fatty stools. Given the characteristic manifestations of choledocholithiasis, it is important to seek medical attention in a timely manner for further diagnosis and treatment.
- Pain in the right upper quadrant of the abdomen: often occurs after eating and may be accompanied by nausea and vomiting.
- Jaundice: caused by bile stagnation and manifested by yellowing of the skin, mucous membranes, and sclera of the eyes.
- Itchy skin: may be associated with impaired liver function due to gallstone disease.
- Dark urine: may be a result of obstruction of the bile ducts due to stones in the bile ducts.
- Discolored or fatty stools: changes in stool may be a consequence of digestive disturbances due to bile stagnation.
The perspective of medical professionals on the treatment of choledocholithiasis.
Medical specialists consider the treatment of choledocholithiasis as a comprehensive process that may include conservative methods, medication, and surgical intervention. To date, there are several approaches to treating this condition, and the choice of method depends on the characteristics of the stones, the degree of blockage in the bile ducts, as well as the overall condition of the patient.
Experts generally recommend starting the treatment of choledocholithiasis with conservative measures, such as a low-fat diet and drug therapy to improve the functioning of the biliary system. In cases where conservative methods prove insufficiently effective or complications arise, surgical removal of stones from the bile ducts may be necessary. Experts emphasize the importance of an individualized approach to treatment, taking into account the unique clinical picture and potential risks for each patient.

Methods for diagnosing choledocholithiasis
For the diagnosis of choledocholithiasis, various methods may be used, including ultrasound (US), computed tomography (CT) of the abdomen, and magnetic resonance cholangiography (MRCP). Ultrasound of the bile ducts is one of the most accessible and informative methods for detecting stones in the bile duct. Other methods, such as MRCP and endoscopic retrograde cholangiopancreatography (ERCP), can be used for more detailed visualization of the bile ducts and determining further treatment strategies.
Additionally, the attending physician may recommend biochemical blood and urine tests to assess liver function and confirm the presence of inflammatory processes or jaundice associated with choledocholithiasis. Clinical manifestations, in conjunction with the results of diagnostic studies, allow for the determination of the presence and degree of disease progression and contribute to the selection of the optimal treatment strategy for the patient.
- Ultrasound examination (US): a method that allows visualization of the bile ducts and detection of stones and certain changes in the gallbladder.
- Computed tomography (CT): provides a more detailed image of the abdominal area, helping to identify stones in the bile ducts and assess the condition of surrounding tissues.
- Magnetic resonance cholangiography (MRCP): allows non-invasive visualization of the bile ducts, identification of stones, and assessment of the condition of the gallbladder.
- Biochemical blood and urine tests: help to assess liver function, presence of inflammation, and jaundice associated with choledocholithiasis.
- Endoscopic retrograde cholangiopancreatography (ERCP): an invasive method for diagnosing and performing therapeutic manipulations in the biliary tract.
Cholodocholithiasis Therapy
Surgical treatment of choledocholithiasis may involve endoscopic retrograde cholangiopancreatography (ERCP) with stone removal from the bile ducts using endoscopic instruments. In the case of large or complex stones, cholecystectomy may be necessary to remove the gallbladder. The optimal treatment method is determined on an individual basis depending on clinical data, the severity of complications, and the overall condition of the patient.
- Conservative treatment: Includes the use of medications to dissolve bile, alleviate pain, and control inflammation and infection.
- Endoscopic retrograde cholangiopancreatography (ERCP): Conducted to remove bile stones from the ducts using endoscopic methods.
- Cholecystectomy: Surgical removal of the gallbladder may be necessary in cases of complicated or large stones.
- Anti-inflammatory therapy: Used to reduce inflammation in the bile ducts and surrounding tissues.
- Diet and lifestyle recommendations: Include consuming healthy foods, controlling weight, and engaging in moderate physical activity to reduce the risk of stone formation.
Preventive measures for choledocholithiasis
Other key preventive measures include regular intake of dietary fiber, limiting alcohol consumption, avoiding prolonged fasting, and following the doctor’s recommendations in the presence of risk factors for the development of choledocholithiasis. Regular medical check-ups and monitoring of bile parameters also play an important role in the timely detection and prevention of this disease.
- Maintaining a healthy lifestyle, including moderate physical activity and a balanced diet.
- Limiting the intake of fats and simple carbohydrates, and including vegetables, fruits, and whole grains in the diet.
- Regular consumption of dietary fibers to support a healthy biliary system.
- Avoiding excessive alcohol consumption, prolonged fasting, and maintaining weight control.
- Regular medical check-ups to identify risk factors and maintain the health of the bile ducts.
Amazing Aspects of Choledocholithiasis
Another interesting fact about choledocholithiasis is that preventive measures, such as a balanced diet and moderate physical activity, can significantly reduce the risk of developing this condition. This allows individuals to take an active role in maintaining the health of their biliary system and decreasing the likelihood of complications associated with choledocholithiasis.