Cholecystopancreatitis: symptoms, causes, and treatment
- Description of cholecystopancreatitis
- Etiology of cholecystopancreatitis
- Clinical picture of cholecystopancreatitis
- Expert opinions on the treatment of cholecystopancreatitis
- Diagnosis of cholecystopancreatitis
- Treatment of cholecystopancreatitis
- Prevention of cholecystopancreatitis
- Amazing aspects of cholecystopancreatitis
- FAQ
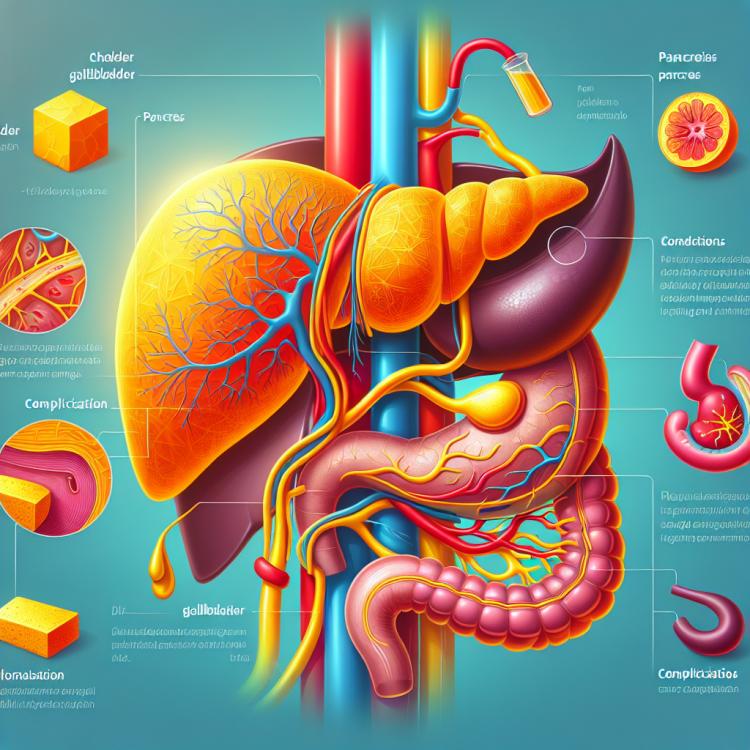
Description of cholecystopancreatitis
Cholecystopancreatitis is an inflammatory process affecting both the gallbladder and the pancreas. This pathology is often caused by the formation of stones in the gallbladder, which can block the bile ducts and lead to inflammation. Symptoms of cholecystopancreatitis include abdominal pain, nausea, vomiting, fever, and changes in bowel movements.
The diagnosis of cholecystopancreatitis usually involves laboratory tests, ultrasound, computed tomography, or magnetic resonance imaging. Treatment of this condition may include conservative methods such as prescribing anti-inflammatory medications and dietary changes, or surgical intervention, including the removal of the gallbladder or stones.
Etiology of cholecystopancreatitis
The etiology of cholecystopancreatitis is usually associated with the formation of gallstones, which can block the bile ducts and cause inflammation. Other causes include infections of the gallbladder or pancreas, as well as anomalies of the biliary tract. Various factors such as diet, genetics, and medication can also contribute to the development of this disease.
- Gallstones: The formation of gallstones can block the bile ducts, leading to inflammation of the gallbladder or pancreas.
- Infections: The gallbladder or pancreas can become inflamed due to bacterial or viral infection.
- Abnormalities of the bile tract: Various congenital or acquired abnormalities of the bile ducts can predispose to the development of cholecystopancreatitis.
- Diet: Overeating fatty and fried foods, as well as prolonged fasting, can contribute to the development of the disease.
- Genetics: Hereditary factors may influence an increased tendency to form gallstones or disorders in the bile tract, which can lead to cholecystopancreatitis.
Clinical picture of cholecystopancreatitis
The clinical picture of cholecystopancreatitis may include symptoms such as pain in the upper abdomen, especially in the right hypochondrium, which may radiate to the back. Patients may experience nausea, vomiting, jaundice of the skin and sclera, as well as general weakness. In the case of the acute form of the disease, signs of a systemic inflammatory response may be observed, such as increased body temperature and rapid heartbeat, requiring urgent medical intervention.
- Abdominal pain in the upper abdomen: One of the main symptoms of cholecystopancreatitis is sharp or dull pain in the right upper quadrant, often radiating to the back.
- Nausea and vomiting: Patients may experience nausea, vomiting, and abdominal discomfort, especially after eating.
- Jaundice of the skin and sclera: In case of obstruction of the bile ducts, patients may develop jaundice of the skin and sclera, caused by excessive deposition of bile pigments.
- General weakness: Feelings of fatigue, weakness, and loss of appetite are often observed in patients with cholecystopancreatitis, especially during exacerbation periods.
- Systemic inflammatory response: The acute form of cholecystopancreatitis may be accompanied by elevated body temperature, increased heart rate, and other signs of inflammation requiring immediate intervention by a medical professional.
Expert opinions on the treatment of cholecystopancreatitis
Expert opinions on the treatment of cholecystopancreatitis emphasize the importance of an individual approach for each patient based on the characteristics of the disease, the overall condition of the body, and possible complications. Experts typically recommend a comprehensive approach that includes medication, diet, physical exercises, and in some cases, surgical intervention. The main principle of treatment is to eliminate the causes of cholecystopancreatitis, reduce inflammation, and prevent relapses of the disease.

Diagnosis of cholecystopancreatitis
The diagnosis of cholecystopancreatitis includes a comprehensive set of methods, starting with the patient’s history and physical examination, and continuing with laboratory tests such as blood tests for inflammatory markers and pancreatic enzymes. Instrumental methods are used to confirm the diagnosis, including ultrasound, computed tomography, and magnetic resonance imaging of the abdominal cavity, which allow for the assessment of the condition of the gallbladder, pancreas, and surrounding tissues. Accurate diagnosis plays a key role in determining the treatment strategy and prognosis for patients with cholecystopancreatitis.
- Medical history and physical examination: The doctor conducts a detailed study of the patient’s medical history and examination to assess clinical signs.
- Laboratory tests: Blood tests for levels of inflammatory markers, leukocytes, and pancreatic enzymes aid in the diagnosis of cholecystopancreatitis.
- Ultrasound examination: A non-invasive method that allows visualization of abdominal organs, including the gallbladder and pancreas.
- Computed tomography (CT) of the abdomen: An examination using X-rays and computer image processing to obtain a more detailed picture of the condition of the organs.
- Magnetic resonance cholangiopancreatography (MRCP): A diagnostic method that assesses the condition of the bile ducts and pancreas using magnetic resonance.
Treatment of cholecystopancreatitis
- Conservative treatment: Includes fasting, intravenous fluid administration, antibiotics to fight infection, and pain relief medications to reduce pain.
- Surgical treatment: In case of complications, surgery may be required, such as cholecystectomy (removal of the gallbladder) or drainage of the pancreas.
- Diet therapy: A special diet aimed at reducing the load on the digestive system is an important component of comprehensive treatment.
- Check-up examinations: It is important to regularly undergo examinations and consultations with specialists to monitor the condition and effectiveness of treatment.
- Rehabilitation: After treatment, rehabilitation is important, which includes physical activity, adherence to dietary recommendations, and therapeutic procedures for health recovery.
Prevention of cholecystopancreatitis
For people at increased risk of developing the disease, such as those who are obese or have a family history of cholecystopancreatitis, it is important to undergo regular medical examinations and monitor their health. Early detection and control of factors contributing to the development of the disease help prevent serious complications and ensure the long-term preservation of digestive organ function.
- Healthy eating: Including foods rich in fiber, low in fat, and with moderate sugar content helps maintain the health of the digestive system.
- Regular physical activity: Moderate exercise regularly helps reduce the risk of developing cholecystopancreatitis and other diseases.
- Quitting smoking and alcohol: Avoiding the negative effects of nicotine and alcohol on the digestive organs helps prevent diseases, including cholecystopancreatitis.
- Maintaining a healthy weight: Fighting excess weight reduces the risk of gallstone formation and the development of pancreatitis.
- Regular medical check-ups: Control examinations help detect early signs of disease and take necessary preventive measures against cholecystopancreatitis.
Amazing aspects of cholecystopancreatitis
Research in the field of cholecystopancreatitis continues to expand our knowledge of its mechanisms of development and effective treatment methods. New diagnostic technologies and surgical interventions are gradually changing the approach to treating patients with this disease, opening new prospects in the field of medicine for the future.