Intestinal obstruction: symptoms, diagnosis, and treatment methods
- Understanding Intestinal Obstruction: Key Aspects
- Etiology of intestinal obstruction
- The clinical picture of intestinal obstruction
- Expert opinion on treating intestinal obstruction
- Methods of diagnosing intestinal obstruction
- Main methods of treating intestinal obstruction
- Prevention measures for intestinal obstruction
- Amazing Aspects of Intestinal Obstruction
- FAQ
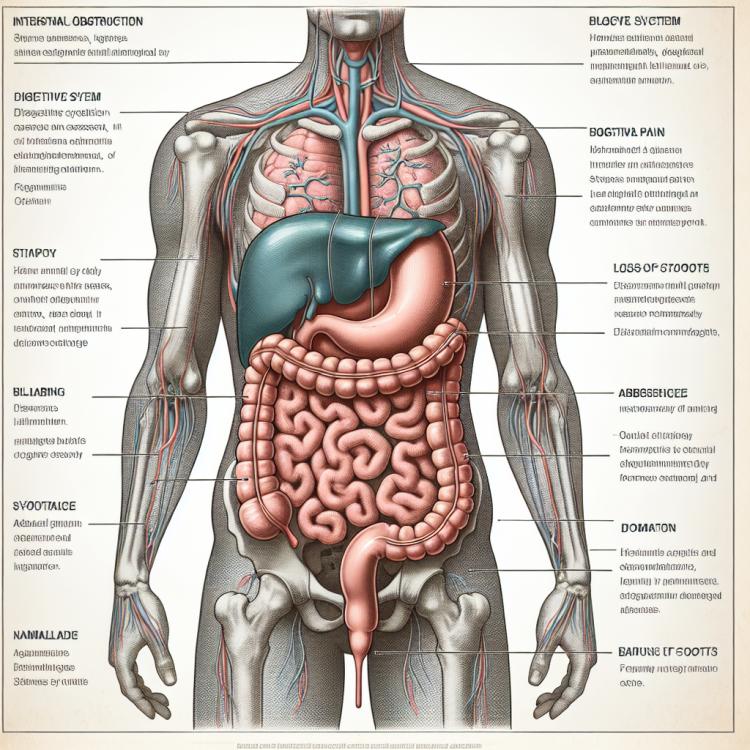
Understanding Intestinal Obstruction: Key Aspects
Intestinal obstruction, or bowel obstruction, is a condition characterized by the disruption of the normal passage of contents through the gastrointestinal tract. The main cause of intestinal obstruction may be a mechanical blockage caused by tumors, intestinal adhesions, intra-abdominal adhesions, or hernias, or a functional disorder such as spasms or paralysis of the intestine, which leads to impaired motility and peristalsis of the gastrointestinal tract.
In intestinal obstruction, characteristic symptoms occur, such as severe abdominal pain, absence of gas and stool, as well as nausea and vomiting. To diagnose this condition, a clinical examination is necessary, including medical history, physical examination, and instrumental diagnostic methods such as X-rays and computed tomography. Treatment of intestinal obstruction focuses on eliminating the cause and restoring normal bowel patency, often requiring surgical intervention.
Etiology of intestinal obstruction
Intestinal obstruction can have various causes, including mechanical barriers, decreased peristalsis, inflammatory processes, tumors, and other pathologies. Mechanical causes, such as compression of the intestine by a tumor or a foreign body, are one of the primary reasons for intestinal obstruction. Inflammatory diseases, such as chronic colitis, Crohn’s disease, or diverticulitis, can also lead to impaired intestinal passage.
Other factors, including intestinal ischemia, circulation disorders, as well as certain neurological and metabolic conditions, can contribute to the development of intestinal obstruction. Understanding the etiology of this condition plays an important role in choosing the optimal treatment strategy and allows specialists to effectively combat this disease.
- Mechanical causes: include intestinal tumors, foreign bodies, strictures, and other obstructions that can block the intestinal lumen.
- Inflammatory diseases: such as Crohn’s disease, ulcerative colitis, and others, can lead to inflammation of the intestines and worsen its permeability.
- Circulatory disorders: intestinal ischemia or other circulation problems can lead to tissue necrosis and obstruction of the intestines.
- Infections: certain infections, especially those that cause significant inflammation or tissue growth, can be a cause of intestinal obstruction.
- Neurological and metabolic conditions: such as Hirschsprung’s disease, diabetic neuropathy, and other neurological or metabolic disorders can also contribute to the development of intestinal obstruction.
The clinical picture of intestinal obstruction
The clinical picture of intestinal obstruction includes a variety of symptoms that can be caused by both intestinal obstruction and impaired permeability. Patients often complain of severe abdominal pain, the need for vomiting, stool disorders, abdominal bloating, as well as a possible absence of gases and intestinal sounds. In addition, signs of general body intoxication may be observed in cases of intestinal obstruction, such as fever, weakness, loss of appetite, and weight loss.
It is important to note that the symptoms of intestinal obstruction may vary depending on the cause and level of intestinal damage. Studying the clinical picture and identifying the main symptoms help doctors diagnose the condition, assess its severity, and choose the most effective treatment methods.
- Severe abdominal pain: often there is cramping or sharp pain in the abdomen that can occur suddenly.
- Need to vomit: patients may experience a strong sense of nausea, which can lead to vomiting as an attempt by the body to eliminate the problem.
- Bowel disorders: changes in the frequency and nature of bowel movements, including constipation or diarrhea, can be signs of intestinal obstruction.
- Abdominal distension: patients often experience swelling and an increase in abdominal volume, which is related to impaired peristalsis and gas formation.
- Absence of gas and intestinal sounds: in case of intestinal obstruction, there may be a lack of passage of gas and absence of peristaltic sounds when listening to the abdomen.
Expert opinion on treating intestinal obstruction
Expert opinion on the treatment of intestinal obstruction reflects the importance of fundamental principles of therapy for this condition. Medical experts emphasize that the first step must be to eliminate the cause of the obstruction, whether it is surgical intervention to remove tumors or other blockages, or conservative treatment to address inflammatory processes in the intestines.
Furthermore, experts recommend a comprehensive approach to treatment that includes medication therapy, diet, physiotherapy, and rehabilitation measures. An individualized approach to each patient, taking into account their condition, age, causes, and severity of the disease, plays a key role in the successful treatment of intestinal obstruction and minimizing the risks of complications.

Methods of diagnosing intestinal obstruction
The diagnosis of intestinal obstruction involves a comprehensive approach and the use of various methods. The main diagnostic methods include a clinical examination of the patient, history taking, and physical examination. Radiological studies, such as abdominal X-ray, barium studies, and computed tomography (CT), can help identify the cause and location of the intestinal obstruction. Endoscopic methods, such as colonoscopy or esophagogastroduodenoscopy, can also be employed for a more detailed examination of the bowel condition.
Additional diagnostic methods, such as ultrasound examination, are useful in assessing the condition of tissues and the volume of fluid in the abdominal cavity. Laboratory tests of blood and urine can complement the overall picture of the disease and assist in evaluating the patient’s general condition. Accurate and timely diagnosis of intestinal obstruction allows specialists to prescribe optimal treatment and prevent possible complications.
- Clinical examination and history: The expert conducts a thorough examination of the patient, identifying the characteristics of abdominal pain, the presence of vomiting, changes in bowel function, and other symptoms.
- Radiological studies: X-ray of the abdomen, barium studies, and computed tomography (CT) help visualize the structure of the intestine and identify the cause of the obstruction.
- Endoscopic methods: Colonoscopy, esophagogastroduodenoscopy, and other endoscopic studies allow for a more detailed examination of the condition of the intestine from the inside.
- Ultrasound examination: This method helps assess the condition of the tissues and determine the presence of fluid in the abdominal cavity, which is important for diagnosing intestinal obstruction.
- Laboratory tests: Blood and urine tests can reveal possible pathologies, assess the overall condition of the patient, and provide additional data for diagnosing intestinal obstruction.
Main methods of treating intestinal obstruction
After treatment, it is important to monitor the patient, assess their condition, and evaluate the effectiveness of the measures taken. Cooperation among doctors of various specialties, including surgeons, gastroenterologists, anesthesiologists, and other specialists, allows for the selection of the optimal treatment path and ensures the patient receives qualified medical care.
- Conservative therapy: includes taking medications to reduce inflammation, relieve pain and spasms, and normalize intestinal activity.
- Surgical intervention: if necessary, involves surgical removal of the obstruction, resection of the affected intestinal segment, or restoration of its integrity.
- Supportive therapy: may include infusion therapy, antibiotics, correction of electrolyte and fluid disturbances, as well as other procedures to maintain the overall condition of the body.
- Diet and nutrition: the prescription of a special diet and dietary recommendations plays an important role in restoring normal intestinal function and easing the treatment process.
- Rehabilitation and rehabilitative therapy: after treatment, it is important to carry out follow-up monitoring, physiotherapy, and other rehabilitation activities to restore body functions.
Prevention measures for intestinal obstruction
Preventing possible causes of intestinal obstruction, such as controlling chronic diseases, properly using medications, stabilizing the condition of postoperative scars, or organizing a rational diet for intestinal diseases, is of significant importance for preventing this pathological condition. Regular medical check-ups, especially for patients at increased risk, as well as following the physician’s recommendations, will help reduce the likelihood of developing intestinal obstruction.
- Healthy eating: Regular consumption of foods rich in dietary fiber helps maintain intestinal health and contributes to normal peristalsis.
- Consuming enough liquid: Drinking an adequate amount of water throughout the day helps improve digestion and prevents constipation, which can contribute to the formation of intestinal obstruction.
- Physical activity: Regular physical exercise helps improve intestinal motility and prevents sluggish peristalsis, which can lead to obstruction.
- Avoiding harmful habits: Quitting smoking and moderate alcohol consumption contribute to overall body health, including the condition of the intestines.
- Managing chronic diseases: Regularly following the doctor’s recommendations and taking medications as prescribed helps prevent exacerbations of diseases that can lead to intestinal obstruction.
Amazing Aspects of Intestinal Obstruction
Another interesting aspect is the variety of diagnostic and treatment methods for intestinal obstruction, which continue to evolve due to modern technologies and scientific research. Understanding the mechanisms of this disease and the ongoing improvement of treatment methods open new horizons in medical practice and contribute to better therapy outcomes for patients.