Leukoplakia of the vulva: diagnosis, complications, and prevention
- Understanding Vulvar Leukoplakia
- Etiology of Vulvar Leukoplakia
- The main symptoms of vulvar leukoplakia
- Expert opinion on the treatment of vulvar leukoplakia
- Methods of diagnosing vulvar leukoplakia
- Main methods of treatment for vulvar leukoplakia
- Prevention measures for vulvar leukoplakia
- Interesting aspects of vulvar leukoplakia
- FAQ
Understanding Vulvar Leukoplakia
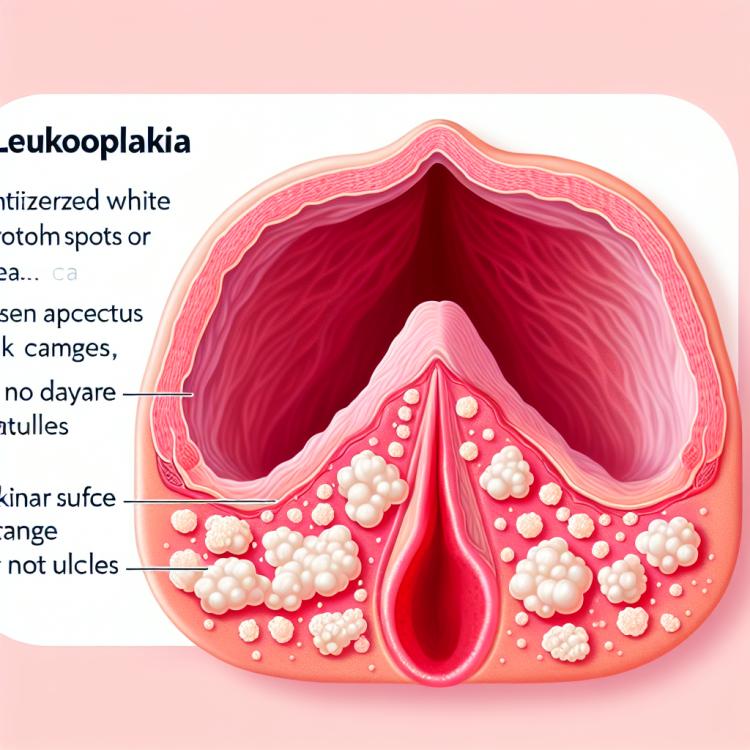
Leukoplakia of the vulva is a precancerous pathological condition characterized by the formation of whitish spots or plaques on the mucous membrane of the vulva. These changes may be associated with prolonged irritation or trauma to the skin, as well as with genetic or immunological factors. The study of leukoplakia of the vulva is important for the proper diagnosis and treatment of women suffering from this pathological condition.
Understanding leukoplakia of the vulva requires a comprehensive approach, including clinical assessment, histological examination of biopsy material, and consideration of individual patient characteristics. Additionally, it is important to track the dynamics of the process and respond promptly to changes in clinical symptoms. A thorough study of medical literature and the practical experience of specialists allows for a deeper understanding of the mechanisms of development and the risk factors of this disease.
Etiology of Vulvar Leukoplakia
The etiology of vulvar leukoplakia is multifactorial. The main causes of this disease can be chronic trauma to the mucous membrane of the vulva, viral infections (including the human papillomavirus), prolonged exposure to harmful chemicals, as well as factors related to smoking. Disorders in the immune system may also contribute to the development of vulvar leukoplakia, highlighting the importance of a comprehensive approach to the treatment and prevention of this disease.
- Chronic trauma to the vulvar mucosa: Ongoing trauma caused by mechanical irritants can contribute to the development of leukoplakia.
- Viral infections: Viral exposure, including human papillomavirus (HPV), can be one of the causes of vulvar leukoplakia.
- Exposure to harmful chemicals: Prolonged contact with aggressive chemicals can cause changes in tissues and lead to the formation of leukoplakia.
- Tobacco smoking: Tobacco smoke contains many carcinogens that can adversely affect vulvar cells, promoting the appearance of leukoplakia.
- Immune system disorders: Weakened immunity can make the body more susceptible to the development of vulvar leukoplakia, as immune defense mechanisms do not function properly.
The main symptoms of vulvar leukoplakia
The main symptoms of vulvar leukoplakia include the appearance of white, gray, or yellowish spots or plaques on the surface of the vulvar mucosa. These changes may be accompanied by itching, burning, and discomfort in the genital area. Symptoms often intensify upon contact with urine, clothing, or during sexual intercourse. For an accurate diagnosis and assessment of the extent of the condition, it is important to consult a specialist and undergo regular examinations.
More pronounced symptoms can also occur, such as bleeding, ulcers, and sores on the surface of the vulva. Some patients may experience painful sensations during urination or unusual discharge from the genital tract. If such symptoms are present, it is important not to delay a visit to the doctor for timely diagnosis and treatment.
- Appearance of white, gray, or yellowish spots or plaques on the surface of the vulva: such changes are often the first sign of vulvar leukoplakia and require careful monitoring.
- Itching, burning, and discomfort in the genital area: these symptoms may be related to changes in the mucous membranes and hinder normal daily activities.
- Worsening of symptoms upon contact with urine, clothing, or during sexual intercourse: increased sensitivity and irritation with physical impact may be characteristic signs of vulvar leukoplakia.
- Bleeding, ulcers, and sores on the surface of the vulva: more advanced cases of leukoplakia may be accompanied by bleeding and ulcers that require specialized treatment.
- Painful sensations during urination or unusual discharge from the genital tract: such symptoms may indicate further progression of the disease and require a doctor’s consultation.
Expert opinion on the treatment of vulvar leukoplakia
Expert opinions on the treatment of vulvar leukoplakia emphasize the importance of an individualized approach for each patient. Specialists recommend a combined approach, including both conservative treatment methods and surgical interventions depending on the extent of the lesion and the symptoms of the disease. Local application of medications, physiotherapy, as well as regular monitoring by a doctor help control the condition of the disease and minimize risks.
Experts also point out the necessity of regular screening and preventive measures for women at increased risk of developing vulvar leukoplakia, including careful monitoring and timely medical consultations. An important aspect is the trusting relationship between the patient and the doctor, which contributes to effective diagnosis and treatment of the disease, ensuring optimal results and quality of life for the patient.

Methods of diagnosing vulvar leukoplakia
Diagnosis of vulvar leukoplakia usually includes a visual examination of the vulva and a biopsy of the affected area for subsequent cytological and histological analysis. Cellular examination will help determine the presence of pathological changes in the tissues of the vulva and identify possible dysplastic changes, which are necessary for establishing an accurate diagnosis.
To clarify the extent of the process, colposcopy may be used – a diagnostic method that allows visualization of the mucous membrane of the vulva under magnification using a special device. Conducting magnetic resonance imaging (MRI) may be necessary in case of suspicion of the process spreading to adjacent tissues or organs.
- Visual inspection: the primary diagnostic method, involving a careful look at the surface of the vulva to detect white, gray, or yellowish spots.
- Biopsy: the procedure of collecting a tissue sample for cytological and histological analysis to identify pathological changes.
- Colposcopy: a diagnostic method that allows the doctor to magnify the image of the vaginal mucosa for a more detailed examination.
- Cytological analysis: the study of cells from the biopsy sample under a microscope to identify abnormalities or dysplasia.
- Magnetic resonance imaging (MRI): a diagnostic method that can be used to assess the extent of the process beyond the vulva.
Main methods of treatment for vulvar leukoplakia
In cases of pronounced disease dynamics or the presence of dysplastic changes, surgical intervention, such as excision of the affected tissues, may be recommended. It is important to consult a doctor for an individualized treatment approach and to follow the specialist’s recommendations to achieve the best results.
- Topical therapy: prescribing creams or ointments with glucocorticosteroids to reduce inflammation and itching in the affected vulvar area.
- Procedures of cryodestruction and laser therapy: removal of affected areas to improve the condition of the mucous membrane.
- Surgical intervention: excision of affected tissues may be recommended in the presence of dysplastic changes and pronounced disease dynamics.
- Systemic therapy: the use of oral medications to enhance the treatment effect and address the underlying processes of leukoplakia.
- Following specialist recommendations: it is important to have regular examinations, monitor the dynamics of the condition, and strictly adhere to all physician’s instructions for effective treatment of vulvar leukoplakia.
Prevention measures for vulvar leukoplakia
Another important aspect of prevention is avoiding exposure to aggressive substances in the vulvar area, including chemicals that can cause irritation or damage to the mucous membrane. Adhering to a healthy lifestyle, engaging in regular physical activity, proper nutrition, and appropriate intimate hygiene can also contribute to the prevention of vulvar leukoplakia.
- Regular check-ups with a gynecologist to detect pathological changes in the vulva area.
- Avoiding smoking, as tobacco exposure can contribute to the development of leukoplakia.
- Maintaining proper hygiene of the genital area and using soft underwear made of natural materials.
- Avoiding exposure to aggressive chemicals in the vulva area to prevent irritation or damage to the mucous membrane.
- Adopting a healthy lifestyle, including regular physical exercise, proper nutrition, and correct intimate hygiene to reduce the risk of developing vulvar leukoplakia.
Interesting aspects of vulvar leukoplakia
Another interesting fact is that the presence of vulvar leukoplakia may increase the risk of developing vulvar cancer. Therefore, it is important to conduct regular monitoring of the vulva and promptly consult a doctor for diagnosis and effective treatment, which can help prevent possible complications.