Uterine leiomyoma: diagnosis, types, and treatment methods
- Official statistics and facts about uterine leiomyoma
- Hormonal and genetic triggers for the development of uterine leiomyoma
- Identification of uterine leiomyomas: key signs and manifestations
- The position of experts on the methods for treating uterine leiomyoma
- Modern methods of diagnosing uterine leiomyoma
- Innovative approaches to the treatment of uterine leiomyoma
- Prevention measures for uterine leiomyoma
- Interesting aspects of uterine leiomyomas
- FAQ
Official statistics and facts about uterine leiomyoma
Uterine leiomyoma, also known as uterine fibroid, is the most common benign tumor in women of reproductive age. Its exact cause is still not studied, however, it is believed that hormonal changes, genetic factors, and uterine growth may contribute to the development of this condition. The incidence of uterine leiomyoma significantly depends on the age of patients; for instance, its prevalence among women aged 30-40 years is about 20%, while for women aged 50 and older, it is about 50%.
Uterine leiomyoma is more commonly found in women who have certain risk factors, such as early onset of menstruation, Black women, and women with low vitamin D levels. Most uterine leiomyomas do not even show symptoms and are found incidentally during examinations for other reasons. Nevertheless, if clinical manifestations such as menstrual disorders, lower abdominal pain, or increased urination are present, it is advisable to see a doctor for diagnosis and treatment.
Hormonal and genetic triggers for the development of uterine leiomyoma
The development of uterine leiomyoma is due to a complex interaction of various hormonal factors. Prolactin, estrogens, progesterone, and other hormones play a key role in creating an optimal environment for the growth and development of the tumor. Genetic factors also influence the tendency to develop leiomyoma, caused by mutations in certain genes that control cellular division and tissue growth.
Research shows that some women may have a hereditary predisposition to the development of uterine leiomyoma due to inherited genetic mutations. In this case, the combination of hereditary factors and changes in hormone levels may contribute to the onset and growth of uterine leiomyoma.
- Hormonal imbalance: An excess of estrogens and insufficient levels of progesterone can stimulate the growth of leiomyomas.
- Prolactin: High levels of prolactin may contribute to the development of uterine leiomyomas.
- Genetic predisposition: The presence of certain genetic mutations can increase the risk of developing leiomyomas.
- Hereditary factors: The transmission of genetic changes that promote the formation of leiomyomas from relatives can increase the likelihood of the disease.
- Immunological factors: Systemic disorders in the immune system can influence the development and progression of uterine leiomyomas.
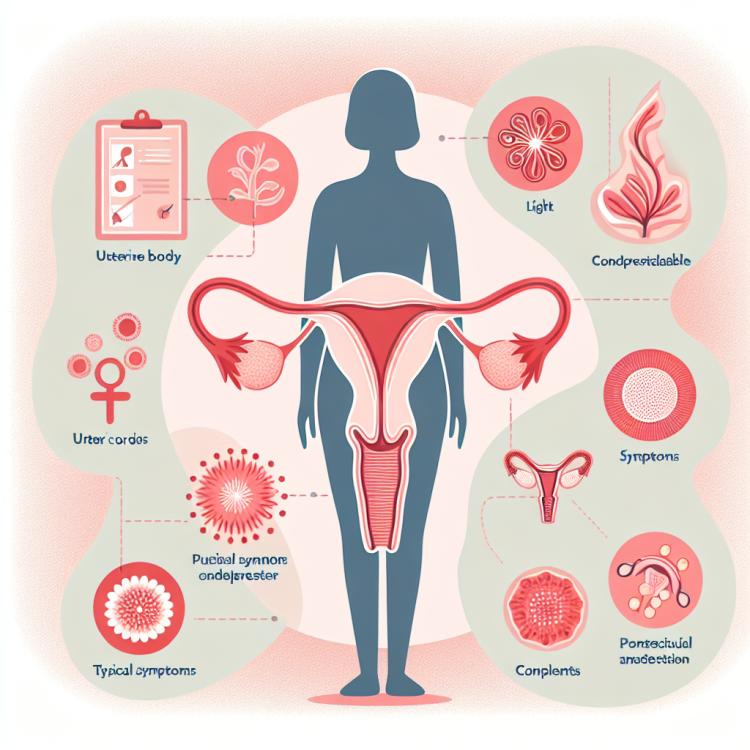
Identification of uterine leiomyomas: key signs and manifestations
Uterine leiomyoma often manifests with various symptoms, including heavy or prolonged menstruation, lower abdominal pain, a feeling of pressure in the pelvis, and changes in urination. Some women may experience pain during sexual intercourse and an increase in abdominal volume due to the tumor’s growth. However, undetected cases of leiomyoma are also found, especially in women without clear clinical manifestations, highlighting the importance of regular medical examinations for the timely detection of this condition.
- Heavy and prolonged menstruation: Uterine leiomyoma can lead to an increase in the volume and duration of discharge.
- Lower abdominal pain: A feeling of discomfort or pain in the abdominal area can be one of the signs of uterine leiomyoma.
- Feeling of pressure in the pelvis: Some women may feel pressure or discomfort in the pelvic area due to the presence of leiomyoma.
- Pain during sexual intercourse: Uterine leiomyoma can cause discomfort or pain during sexual intercourse, which can be one of the signs of its presence.
- Changes in urination: Some women with leiomyoma may experience changes in the frequency or volume of urination, especially if a tumor is putting pressure on the bladder.
The position of experts on the methods for treating uterine leiomyoma
Experts in gynecology and oncology consider various treatment methods for uterine leiomyoma depending on the individual characteristics of the patient, the size of the tumor, its location, and symptoms. In some cases, when the leiomyoma does not cause discomfort and does not negatively affect the body, experts may prefer to monitor the tumor without medical or surgical intervention.
However, in cases where the leiomyoma causes severe symptoms or threatens the patient’s health, experts may recommend surgical removal of the tumor. This can be done either in the form of myomectomy (removal of only the tumor while preserving the uterus) or hysterectomy (complete removal of the uterus). The approach to treating uterine leiomyoma is usually discussed on an individual basis for each patient, taking into account her age, desires to preserve reproductive function, and overall health status.

Modern methods of diagnosing uterine leiomyoma
Modern diagnosis of uterine leiomyoma includes a wide range of methods, such as ultrasound (US), magnetic resonance imaging (MRI), and computed tomography (CT). US is the main method for primary diagnosis of leiomyoma due to its accessibility, safety, and effectiveness. MRI and CT provide more detailed information about the tumor’s structure, its size, and distribution within the uterus, which aids in determining the treatment strategy.
To accurately identify leiomyoma and assess its characteristics, specialists may also use hysteroscopy, endometrial biopsy, and other invasive diagnostic methods. The comprehensive use of various methods allows for a more precise determination of the nature of the uterine tumor, identification of possible complications, and development of an individualized treatment plan for each patient.
- Ultrasound examination (US): The main method of primary diagnosis of uterine leiomyoma, allowing to determine the size, number, and location of tumors.
- Magnetic resonance imaging (MRI): Provides a more detailed image of the structure and distribution of leiomyomas in the uterus, helping to define the treatment strategy.
- Computed tomography (CT): Provides information about the sizes of tumors and their relationship with surrounding tissues, which is important for diagnosis and planning surgical intervention.
- Hysteroscopy: An invasive method that allows visualization of the uterine cavity and detection of leiomyoma within the cavity.
- Endometrial biopsy: Used to obtain tissue samples of the endometrium for further examination and detection of possible changes and tumors.
Innovative approaches to the treatment of uterine leiomyoma
Research in the field of leiomyoma treatment technologies is actively ongoing, including the development of new methods such as high-intensity focused ultrasound (HIFU) and focused ultrasound treatment, which represent minimally invasive alternatives to surgical intervention. Continuous research and clinical trials of new treatment methods for leiomyoma aim to find optimal solutions considering effectiveness, safety, and preservation of women’s reproductive health.
- Application of gonadotropin-releasing hormone (GnRH) agonists: This method of conservative therapy blocks the production of estrogens, which helps reduce the growth of leiomyoma.
- Endometrial resection: A surgical procedure aimed at removing only the layer of the uterine mucosa, this innovative method minimizes the loss of reproductive function.
- Uterine artery embolization (UAE): A radical technique that involves artificially blocking blood flow to the leiomyoma in order to reduce its size and alleviate symptoms.
- High-Intensity Focused Ultrasound (HIFU): A modern technique that uses ultrasound for precise targeting of the tumor without surgical intervention.
- Focused ultrasound treatment: An innovative method that utilizes focused ultrasound waves to destroy the tissues of the leiomyoma while preserving the surrounding healthy tissues.
Prevention measures for uterine leiomyoma
Research also indicates the potential role of certain factors, such as hormone levels and hereditary features, in the development of leiomyoma. If there is a family history of this disease, consulting with a gynecologist and a genetic counselor may help in assessing individual risk and developing personalized prevention strategies.
- Regular medical check-ups: Conducting regular check-ups with a gynecologist can help in the timely detection of pathologies, including uterine leiomyoma.
- Healthy lifestyle: Maintaining a healthy lifestyle, including regular physical exercise and a balanced diet, contributes to overall health and may reduce the risk of tumor development.
- Avoiding excessive stress: Managing stress and maintaining psychological well-being can have a positive effect on the body’s condition and the health of the female reproductive system.
- Discussing family history: Women with family cases of uterine leiomyoma are advised to discuss this information with their doctor to assess the individual risk of the disease.
- Avoiding hormonal imbalances: Maintaining hormonal balance can be crucial in the prevention of leiomyoma, so consulting a doctor for menstrual cycle irregularities or other symptoms is important for health maintenance.
Interesting aspects of uterine leiomyomas
Scientific research is focused on finding new methods for the treatment and prevention of leiomyoma, including the use of innovative technologies and approaches. For instance, the potential of pharmacological agents to reduce tumor size or alleviate symptoms is being actively studied. Minimally invasive treatment options are also being explored, which could reduce the risk of complications and shorten recovery time after surgery.