Lumbalization: symptoms, diagnosis, and treatment methods
Understanding Lumbalization
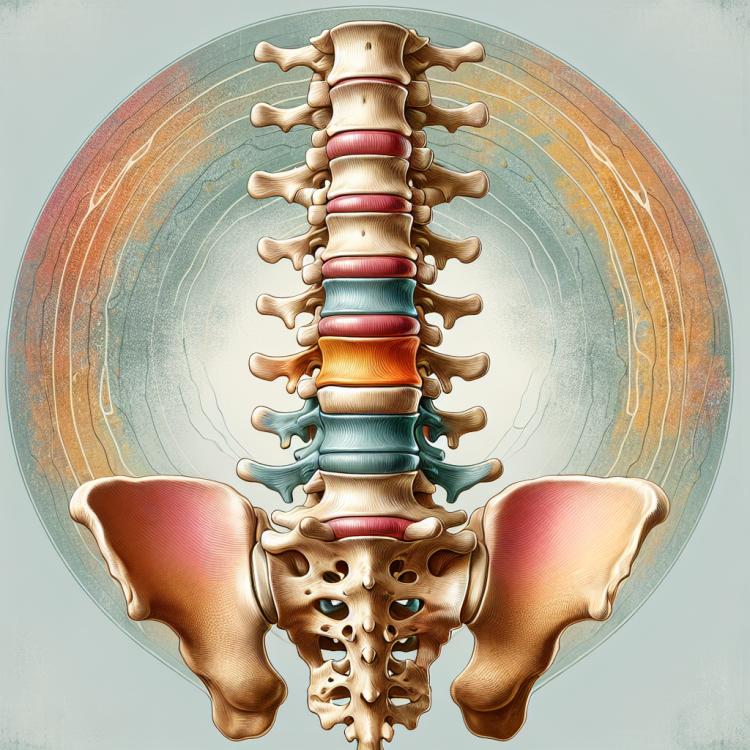
Lumbarization is a congenital developmental disorder of the spine, in which the last lumbar vertebra is lowered to the level of the lumbar region and differs from the norm. This defect may be accompanied by instability of the lumbar spine and compression of nerve structures, causing symptoms such as lower back pain, numbness, and weakness in the lower limbs. Successful management of lumbarization requires accurate diagnosis and an individualized approach to treatment, depending on the symptoms and clinical manifestations in the patient.
Etiology of Lumbarization
Lumbalization is a congenital or acquired condition of the spine characterized by the fusion of the fifth lumbar vertebra with the sacrum. First of all, this process is associated with developmental defects of the spine during embryogenesis, when the full fusion of the fifth lumbar vertebra with the sacrum does not occur. Congenital defects may also be caused by genetic factors or the influence of external toxic substances on the development of the embryonic spine. Acquired causes may include trauma, deformation, or aging processes that lead to developmental abnormalities of the spine.
- Congenital spine development defects: Lumbalization may occur due to incomplete fusion of the fifth lumbar vertebra with the sacral in the embryogenesis period.
- Genetic factors: Some cases of Lumbalization may be attributed to genetic mutations affecting spine development.
- Exposure to toxic substances: External toxins that the mother may encounter during pregnancy can further influence the development of the embryonic spine and contribute to the occurrence of Lumbalization.
- Injuries and deformations: Mechanical damage, such as injuries or deformations in the lumbar spine area, can lead to unusual development of this part of the spine.
- Ageing processes: With age, the muscular and ligamentous apparatus may undergo changes that ultimately can affect the formation of spine structure and contribute to the emergence of Lumbalization.
Clinical picture of Lumbarization
The clinical picture of Lumbalization can manifest various symptoms, depending on the degree and nature of the pathology. Patients often complain of lower back pain radiating down the legs, numbness or weakness in the legs, as well as sensory disturbances. Functional limitations and changes in gait due to spinal deformity are often observed, which can affect the overall quality of life of the patient.
To establish a diagnosis of Lumbalization, it is important to conduct a comprehensive examination, including clinical assessment, X-ray, magnetic resonance imaging (MRI), or computed tomography (CT) of the spine. Treatment of this symptomatic condition may include conservative methods such as physical therapy, therapeutic massage, pharmacotherapy, and in severe cases, surgical intervention may be required.
- Low back pain: patients may experience a variety of pain sensations in the lower back, radiating along the nerves.
- Numbness and weakness in the legs: Lumbarization can cause nerve transmission disorders, leading to numbness and feelings of weakness in the lower limbs.
- Spinal deformity: curvature of the spine and changes in structure can lead to functional limitations and postural disorders.
- Sensory disturbances: patients may experience changes in skin sensitivity, as well as tingling or sensations akin to crawling ants.
- Changes in gait: stiffness of movement and disorders in the function of the lower limbs can lead to changes in gait and overall motor function.
Expert opinion on Lumbarization treatment
Experts in the fields of orthopedics and neurology recommend an individualized approach to the treatment of Lumbarization, taking into account the severity of symptoms, the overall condition of the patient, and the specifics of the disease. In most cases, initial treatment methods include conservative measures such as physiotherapy, exercises to strengthen the back muscles and stretching, as well as the use of anti-inflammatory medications and pain relievers.
In the absence of improvements or in the presence of severe symptoms, surgical intervention may become necessary. Experts emphasize that surgery to correct Lumbarization can improve the functional capabilities of the spine and relieve the patient’s pain syndrome, but it should be considered on a case-by-case basis, taking into account potential risks and benefits.

Diagnosis of Lumbalization
Diagnosis of Lumbalization includes a comprehensive approach for the accurate determination of the condition of the patient’s spinal column. Studying the clinical picture, conducting a physical examination, and measuring the characteristics of pain symptoms are the primary steps in diagnosing this syndrome. Accurate determination of the site and degree of fusion of the fifth lumbar vertebra with the sacrum is carried out using various imaging methods, such as X-ray, computed tomography (CT), and magnetic resonance imaging (MRI). Additional studies, such as electromyography and neuroimaging, may be used to assess the functional state of the nervous system in the lumbar spine area and adjacent tissues.
- Clinical examination: the doctor conducts an examination and interviews the patient to identify the characteristics of pain symptoms and functional limitations.
- X-ray: an X-ray study to visualize the structure of the spine and identify anomalies in the intervertebral discs and joints.
- Computed tomography (CT): the use of X-rays and computer processing to obtain three-dimensional images of the spine and surrounding tissues.
- Magnetic resonance imaging (MRI): the use of magnetic fields and radio waves to create detailed images of the structures of the spine, allowing for the detection of defects and disorders.
- Electromyography: a study of the electrical activity of muscles to assess the functional state of the nervous system and check for neuromuscular disorders.
Treatment of Lumbarization
In cases where conservative methods have not yielded the desired effect or severe complications have arisen, surgical intervention may be necessary. Surgical treatment of Lumbarization may include decompression of the spinal canal, spinal stabilization, or other procedures aimed at preventing further damage and improving the patient’s quality of life. Each case requires an individual approach taking into account the patient’s characteristics and the specifics of the condition.
- Conservative treatment: Includes physiotherapy, therapeutic massage, the use of anti-inflammatory drugs to reduce pain syndrome, and corsets to support the spine.
- Physiotherapeutic exercises: Aimed at strengthening the back muscles, improving flexibility and mobility of the spine.
- Surgical treatment: In cases where conservative methods are ineffective or severe complications arise, surgical intervention may be performed.
- Decompression of the spinal canal: One of the surgical treatment methods aimed at eliminating stenosis and relieving pressure on the nerve structures.
- Spinal stabilization: Another procedure aimed at restoring spinal stability and preventing further damage.
Prevention of Lumbalization
For individuals with a hereditary predisposition to Lumbarization or at risk of developing this condition, it is important to regularly undergo preventive examinations by a specialist and follow recommendations for strengthening the back and maintaining spinal health. Effective prevention of Lumbarization also includes correcting posture, monitoring weight, and engaging in regular physical exercises to strengthen the back muscles and relieve tension from the spine.
- Maintaining a healthy lifestyle: includes moderate physical activity, proper nutrition, avoiding harmful habits, and regular medical check-ups.
- Injury prevention: avoid lifting weights improperly, use correct ergonomics while working, and follow safety measures in sports.
- Posture and weight control: proper posture and weight normalization will help reduce strain on the spine and lower the likelihood of developing lumbar issues.
- Exercises to strengthen back muscles: physical exercise activities are aimed at strengthening the back muscles, which contributes to increased stability of the spine and prevention of degenerative changes.
- Regular medical check-ups: it is important to have regular check-ups with a doctor and monitor the condition of the spine, especially if there are risk factors for lumbar issues.
Interesting Aspects of Lumbarization
Another interesting aspect of Lumbarization is that the diagnosis and treatment of this disease require an individualized approach for each patient. First, it is necessary to accurately determine the cause and nature of the pathology using various imaging methods and functional studies. After that, conservative or surgical treatment may be prescribed depending on the severity of the condition and manifestations in the specific patient.