Mastitis: causes, symptoms, and modern treatment methods.
Understanding mastitis: main aspects and factors
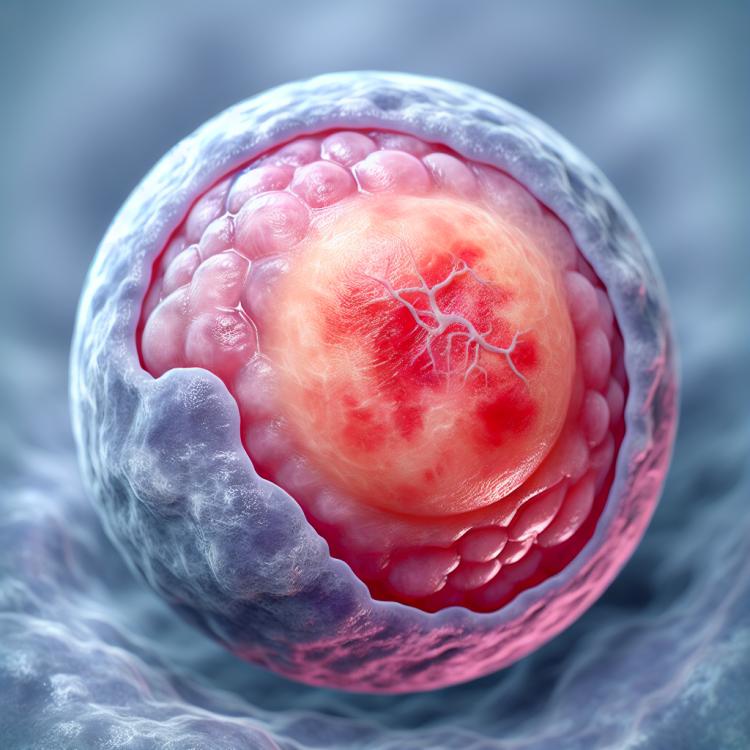
Mastitis is an inflammatory disease of the mammary gland, most often caused by a bacterial infection. The main symptoms of mastitis are pain, swelling, redness, and an increase in temperature in the area of the affected gland. Risk factors include improper feeding, vascular diseases, as well as blood circulation disorders in the mammary gland. Understanding these aspects is important for the diagnosis and successful treatment of this disease.
Risk factors for mastitis development
Mastitis, an inflammatory disease of the mammary gland, can develop under the influence of various risk factors. One of the main factors is infection, most often caused by bacteria. Improper breastfeeding, injuries to the mammary gland, and disturbances in the milk ejection process can also contribute to the development of mastitis. Additionally, the disease is often associated with hygiene violations during feeding, which have a bacterial nature, increasing the likelihood of an inflammatory reaction.
Furthermore, disturbances in the drainage of the mammary gland and increased susceptibility of the body may also contribute to the development of mastitis. Medications that reduce immunity, as well as comorbidities that weaken the body’s defenses, can increase the likelihood of inflammation of the mammary gland. It is important to implement preventive measures, including proper feeding, adherence to hygienic standards, and timely treatment of possible infections, to reduce the likelihood of developing mastitis.
- Infection: the most common cause of mastitis, caused by bacteria or fungi.
- Injuries to the mammary gland: damage, such as from blows or improper feeding, can become entry points for infection.
- Impaired milk flow: milk accumulation in the duct can lead to blockage and infection.
- Poor hygiene during feeding: improper handling, failure to adhere to cleanliness rules during breastfeeding.
- Reduced immunity: factors including stress, poor nutrition, medication can weaken the body’s defense functions.
Primary signs of mastitis
Mastitis is characterized by a variety of clinical manifestations, including inflammation, swelling, and tenderness of the breast. One of the main symptoms is the appearance of redness and warmth on the skin around the affected area, which is associated with inflammation and increased blood flow in that region. Patients may also experience increased pain upon touch or even at rest, which is related to the irritation of nerve endings due to inflammation.
Additionally, discharge from the nipple, changes in the consistency of milk (for example, the presence of thick clots), and general malaise may also be signs of mastitis. Given the variety of symptoms, it is important to seek medical attention at the first signs of possible inflammation of the breast for timely diagnosis and treatment.
- Redness and heat on the skin: the area around the affected breast may become red and hot due to inflammation and increased blood flow.
- Pain and increased discomfort: patients may experience increased pain when touched or at rest, which is associated with irritation of the nerve endings in the inflamed area.
- Nipple discharge: the presence of discharge, especially with traces of pus or blood, may be a sign of mastitis.
- Changes in milk: the consistency of the milk may change, becoming thicker or containing clots, which may also indicate inflammation.
- General malaise: patients with mastitis often feel weakness, fatigue, and general malaise, which complements the clinical picture of the disease.
Expert opinion on the treatment of mastitis
Experts in the field of vascular surgery and gynecology express their opinions on the treatment of mastitis with an emphasis on a comprehensive approach. The individual selection of antibiotics, taking into account the pathogen’s sensitivity to the drug, plays a key role in the effective elimination of the infection. Additionally, there is an emphasis on proper drainage of the breast and the local use of anti-inflammatory agents to reduce swelling and pain.
Experts also highlight the importance of maintaining the overall health of the patient during the treatment of mastitis. Regular examinations and monitoring of the condition of the breasts, adherence to the doctor’s recommendations, and proper breastfeeding are essential parts of successful therapy. An integrated approach, focused on the individual characteristics of the patient and taking into account the specifics of the disease, contributes to a more effective and safe treatment of mastitis.

Methods of diagnosing mastitis
The diagnosis of mastitis may include various methods, starting from clinical examination and medical history to laboratory and instrumental studies. Clinical examination allows for the identification of characteristic signs of inflammation of the mammary gland, including redness, swelling, tenderness, and changes in the discharge from the nipple. An important step is the laboratory study of milk for the presence of bacteria and inflammatory markers, which helps establish the diagnosis and identify the pathogen causing the infection.
Additionally, to confirm the diagnosis, further methods such as mammography or ultrasound examination of the breasts may be performed. These methods allow for the assessment of tissue structure, identification of possible changes, and further confirmation of the presence of inflammatory processes. Careful and comprehensive diagnosis of mastitis plays a key role in determining treatment strategies and preventing possible complications.
- Clinical examination: the doctor conducts a visual examination of the mammary glands and also pays attention to possible changes in the skin and discharge from the nipple.
- Laboratory examination of milk: analysis of milk for the presence of bacteria, inflammatory markers, and other indicators, which helps establish a diagnosis and identify the pathogen.
- Mammography: radiological examination of the mammary glands to assess tissue structure and identify possible changes.
- Ultrasound examination: allows for a more detailed study of the condition of the mammary glands, identifying possible tumors or inflammatory changes.
- Biopsy: in some cases may be performed to obtain a tissue sample and confirm a diagnosis of mastitis.
Approaches to the treatment of mastitis
Additionally, in case of serious complications or lack of effect from conservative treatment, surgical intervention may be required. Surgical methods can be used in the formation of abscesses or other complications that require drainage. It is important to individualize the approach to the treatment of mastitis, taking into account the characteristics of each clinical case and striving to achieve the best results for the patient.
- Use of antibiotics: Antibiotics are often used to eliminate bacteria causing breast infections.
- Anti-inflammatory drugs: Medications in this group help reduce inflammation and alleviate pain.
- Proper feeding: Special attention is given to the correct feeding technique for the child to prevent milk stasis and improve breast drainage.
- Surgical treatment: In cases of complications or lack of effect from conservative treatment, surgical intervention may be required, including the drainage of abscesses and other procedures.
- Individual approach: The treatment strategy should be individualized, taking into account the specifics of each clinical case and based on the requirements of medical tactics.
Measures for the prevention of mastitis
Additionally, regular examinations of the mammary glands by a specialist can help identify early signs of inflammation and initiate treatment in a timely manner. Maintaining a healthy lifestyle, including proper nutrition, regular physical exercise, and avoiding stress, also contributes to strengthening immunity and reducing the likelihood of developing mastitis.
- Proper attachment of the baby to the breast: ensures complete emptying of the mammary gland and prevents milk stasis, which can lead to inflammation.
- Adherence to hygiene standards during feeding: including thorough hand washing before feeding, helps prevent possible infections of the mammary glands.
- Regular breast examinations: allow for the detection of early signs of inflammation and the initiation of treatment at an early stage.
- Healthy lifestyle: including proper nutrition, physical activity, and stress management, contributes to strengthening the immune system and reducing the risk of mastitis.
- Following breastfeeding rules: including the necessity of frequent feeding, a balanced diet for the mother, and avoiding premature weaning, helps in the prevention of mastitis.
Amazing aspects of mastitis
Another interesting aspect of mastitis is its variability of manifestations depending on the individual characteristics of the patient. The variety of clinical forms of symptoms and possible complications makes medical intervention and diagnosis especially important. Thus, studying the remarkable aspects of mastitis contributes to a deeper understanding of this disease and helps develop effective treatment and prevention strategies.