Thrush: understanding symptoms, causes, and treatment methods
Studying candidiasis: main aspects and important information
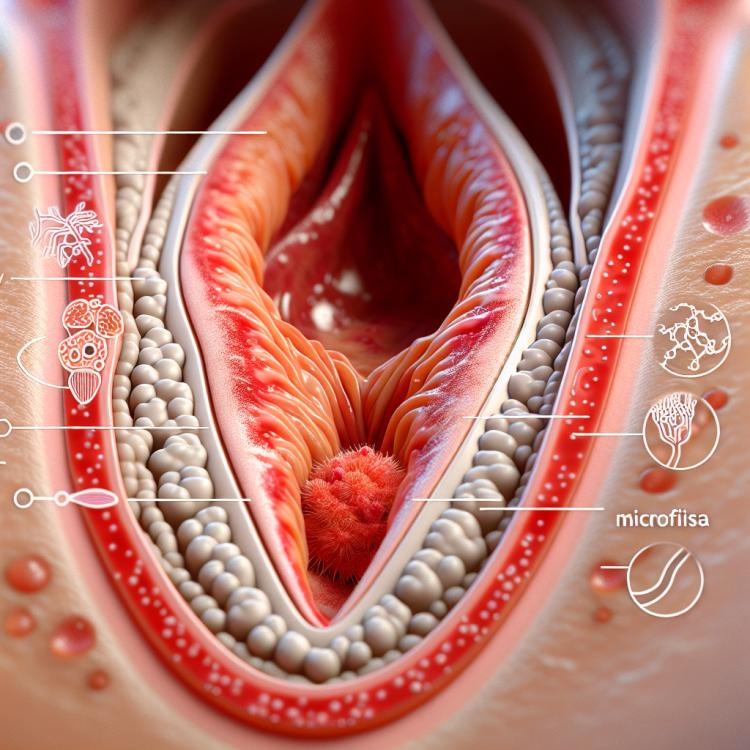
Candidiasis, or vaginal candidiasis, is a common fungal disease in women caused by the fungus Candida. It is characterized by itching, burning, and white discharge. The main risk factors for the development of candidiasis include the use of antibiotics, hormonal changes, diabetes, and immunodeficiency conditions.
Without timely treatment, candidiasis can lead to chronic recurrent forms and complications, such as vaginal dysbiosis or vaginal candidiasis. Comprehensive treatment is of great importance, including the use of antifungal medications, correction of risk factors, and maintaining hygiene measures.
Etiology of candidiasis
Thrush, or vaginal candidiasis, is caused by the fungus Candida albicans, which is usually present in the normal microflora of the vagina. An imbalance of microorganisms in the vagina can be caused by conditions favorable for fungal reproduction, which contributes to the development of thrush.
The etiology of thrush can also be associated with weakened immunity, antibiotic use, hormonal changes, stress, or diabetes. The occurrence of thrush is often related to the disruption of the balance of the vaginal microflora, which creates conditions for the reproduction of fungi and the development of disease symptoms.
- Fungus Candida albicans: the most common cause of thrush, the fungus can reproduce under conditions of imbalance in the vaginal microflora.
- Weakened immunity: a decrease in the body’s protective functions can contribute to the development of thrush.
- Use of antibiotics: the use of antibiotics can disrupt the normal composition of the vaginal microflora, paving the way for fungus reproduction.
- Hormonal changes: fluctuations in hormone levels, for example, during pregnancy or menstruation, can trigger the occurrence of thrush.
- Diabetes: disturbances in glucose levels in the body can contribute to the development of thrush by creating a favorable environment for fungal growth in the vagina.
The clinical picture of thrush
The clinical picture of thrush usually includes symptoms such as itching in the vaginal area, irritation, redness, and swelling around the vulva, as well as an increased amount of discharge, which may be white, clumpy, or have a sour smell. Discomfort or painful sensations in the genital area may occur during urination or sexual contact. In some cases, tenderness and redness in the vaginal mucosa may appear. The development of symptoms is usually associated with a dysbalance of microorganisms in the vagina, which creates conditions for the proliferation of fungi and the manifestation of candidiasis symptoms.
- Itching in the vaginal area: one of the main symptoms of thrush is itching, which may be caused by irritation of the vaginal mucosa.
- Increased discharge: women with thrush often experience a change in the type of discharge, which may be white, thick, or have a sour smell.
- Discomfort during urination: urination with thrush may be accompanied by discomfort or painful sensations in the genital area.
- Pain during sexual intercourse: some women with thrush may experience pain during sexual intercourse due to inflammation of the vaginal mucosa.
- Redness and swelling around the vulva: women with thrush may experience redness and swelling in the vulvar area caused by the inflammatory process.
Expert approach to the treatment of thrush
Experts in the field of gynecology emphasize the importance of a comprehensive approach to treating thrush, which includes not only alleviating symptoms but also correcting factors that contribute to recurrences. Optimal treatment for thrush typically involves the use of antifungal medications to eliminate the fungal infection, as well as the prescription of probiotics to restore normal vaginal microflora.
Experts also recommend paying attention to possible causes of thrush recurrences, such as weakened immunity, microflora imbalance, or hormonal changes, and incorporating the correction of these factors into the overall treatment plan. An individualized approach to each patient and ongoing medical monitoring help achieve effective and long-term control over this condition.

Methods of diagnosing thrush
The diagnosis of thrush usually involves an examination of the vaginal mucosa followed by taking a smear for microscopic examination. This method allows for the detection of the presence of Candida albicans fungi, which are characteristic of thrush. In addition, special laboratory tests, such as culture analyses or DNA testing, are sometimes conducted to accurately confirm the presence of fungi and determine their sensitivity to treatment.
When diagnosing thrush, it may also be important to conduct differential diagnosis with other vaginal infections or sexually transmitted diseases to rule out other possible causes of the symptoms. The doctor may perform an examination and additional tests if the symptoms are not typical of thrush or do not disappear after treatment.
- Visual examination: The doctor examines the vagina and surrounding tissues to identify characteristic symptoms of thrush.
- Sample collection: A sample is taken from the vagina for microscopic examination to determine the presence of Candida albicans fungi.
- Cultural analyses: Laboratory tests, such as culturing fungi from the collected sample, are performed to determine the type of fungi and their sensitivity to treatment.
- DNA testing: This method allows for a more accurate determination of the presence of fungi and their genetic characteristics to select effective treatment.
- Differential diagnosis: Sometimes it is necessary to rule out other vaginal infections or sexually transmitted diseases by conducting a comparative analysis of symptoms and test results.
Approaches to treating candidiasis
In addition to antifungal therapy, probiotics may be prescribed for the treatment of thrush to restore the normal microflora of the vagina. It is also important to avoid potential factors that contribute to the development of thrush, such as wearing overly tight underwear made of synthetic materials or excessive sugar consumption, to reduce the likelihood of recurrent infections.
- Antifungal medications: The use of antifungal drugs, both in the form of local treatment and systemic internal use, to eliminate fungi and cure the infection.
- Probiotics: The prescription of probiotics to restore the normal flora of the vagina after the use of antifungals and to strengthen the body’s protective barrier.
- Avoiding provoking factors: Recommendations for avoiding tight or synthetic underwear, monitoring diet, and reducing sugar intake to prevent recurrences of candidiasis.
- Follow the doctor’s recommendations: It is important to strictly follow the doctor’s instructions regarding the use of medications, dosages, and the duration of the treatment course for effective healing of the infection.
- Comprehensive approach: Often, combined treatment is required, involving the application of several methods and recommendations to achieve complete recovery and reduce the risk of recurrences of candidiasis.
Prevention of thrush
In addition to maintaining hygiene, it is important to strengthen the immune system through healthy eating, physical activity, and stress management. A balanced diet rich in vitamins and minerals helps maintain the body’s protective functions, including protection against fungal infections. Also, regularly check your body for other conditions such as diabetes or changes in hormonal status that may contribute to the development of thrush.
- Compliance with hygiene rules: Regularly wash intimate areas with mild soap, avoid excessive use of detergents, and prevent disruption of the natural balance of microorganisms.
- Wear cotton underwear: Prefer cotton underwear which allows good airflow and helps prevent moisture retention, which can promote fungal growth.
- Strengthening immunity: Maintain a healthy lifestyle, including a balanced diet, physical activity, and stress management, to strengthen immunity and the body’s protective functions.
- Regular medical check-ups: Conduct regular checks and consultations with a doctor to identify and monitor other conditions, such as diabetes or hormonal changes, that may be associated with thrush.
- Avoid tight synthetic underwear: Prefer breathable materials to reduce moisture retention and create less favorable conditions for the growth of Candida albicans fungi.
The unusual side of thrush
Another interesting fact is that women suffering from candidiasis may experience recurrences of the infection. This may occur due to insufficient treatment, non-compliance with hygiene recommendations, or a number of other factors. Therefore, it is important not only to treat candidiasis at its first manifestation but also to follow the doctor’s recommendations to prevent recurrences for maintaining vaginal health.