Heart conduction disorders: symptoms, causes, and treatment
- Basics of Heart Conduction Disorders
- Factors and causes of heart conduction disturbances
- Clinical picture of heart conduction disorders
- Experts’ views on the methods of treating conduction disorders of the heart
- Methods for diagnosing heart conduction disorders
- Methods for treating heart conduction disorders
- Measures to prevent heart conduction disorders
- Engaging aspects of heart conduction disturbances
- FAQ
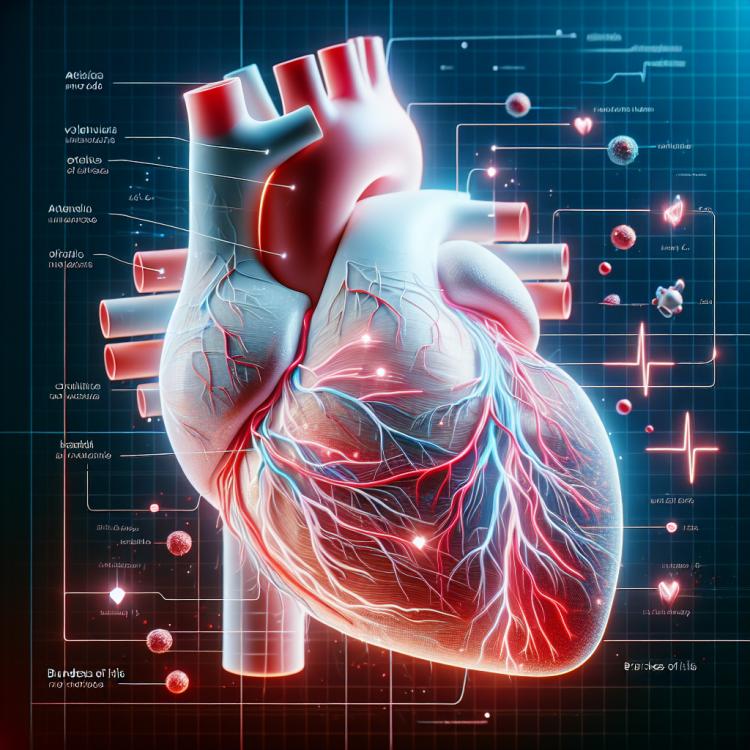
Basics of Heart Conduction Disorders
Disorders of heart conductivity are violations of the electrical activity of the cardiac muscle, which can be caused by various pathological processes. One of the most common types of conductivity disorders is the blockage of the heart’s conduction system, which affects the transmission of impulses between the sections of the heart, potentially leading to serious cardiac complications.
The severity of heart conductivity disorders can vary, and in some cases, additional examinations are required for an accurate diagnosis. Treatment of heart conductivity disorders may include the use of medications; patients with more severe forms of blockage may require the implantation of a pacemaker.
Factors and causes of heart conduction disturbances
Disorders of heart conduction can have various causes, including structural changes in the heart, electrolyte imbalances, the effects of medications, or the presence of conditions such as ischemic heart disease. Other factors contributing to the occurrence of conduction disorders may include congenital anomalies of heart structure or hereditary diseases.
A detailed examination is necessary to identify the underlying causes of heart conduction disorders, which may include ECG, Holter monitoring, echocardiography, and other diagnostic methods. Correction of the underlying disease, prescription of antiarrhythmic medications, implantation of a pacemaker, or surgical interventions are key treatment measures depending on the identified cause of the heart conduction disorder.
- Structural changes in the heart: defects in the structure of the heart can affect its conductivity.
- Electrolyte imbalance: imbalance of minerals such as potassium, sodium, magnesium can influence heart conductivity.
- Medications: certain medications can affect heart conductivity, causing arrhythmias.
- Hereditary factors: congenital heart anomalies and hereditary diseases can be the cause of conductivity disorders.
- Ischemic heart disease: poor blood supply to the heart muscle can lead to conductivity disturbances in the organ.
Clinical picture of heart conduction disorders
Clinical manifestations of heart conduction disorders can be diverse and depend on the specific type of arrhythmia and the degree of conduction impairment. Patients may experience palpitations, rapid heartbeat, the sensation of missed beats, or even syncopal episodes caused by insufficient blood supply to the brain due to heart rhythm disturbances.
Additionally, heart conduction disorders may present changes in the ECG, such as widening of the QRS complexes, asymmetrical increase in R wave, or prolongation of the PR interval. However, for an accurate diagnosis and determination of the type of conduction disorders, examination by a qualified cardiologist using special diagnostic methods is necessary.
- Heartbeat and rapid heartbeat: Patients may experience a sensation of palpitations or rapid heartbeat due to conduction disturbances.
- Sensation of heart skips: The appearance of a sensation of heart skips can be one of the signs of heart conduction disorders.
- Syncopal states: Insufficient blood supply to the brain due to arrhythmias can lead to conditions characterized by loss of consciousness.
- Changes on the ECG: Heart conduction disturbances may manifest as changes in the electrocardiogram, such as widening of QRS complexes or changes in PR intervals.
- Respiratory failure: Some patients with heart conduction disturbances may experience impaired respiratory function due to insufficient blood supply to organs and tissues.
Experts’ views on the methods of treating conduction disorders of the heart
Experts in the field of cardiology identify several main methods for treating heart conduction disorders, depending on the type and severity of the pathology. Among them, pharmacological treatment stands out, which includes the use of antiarrhythmic drugs that normalize heart rhythm and improve the conductivity of cardiac tissue. In some cases, the use of pacemakers may be required to maintain a normal heart rhythm.
In addition to medication therapy, surgical intervention may be needed to correct structural anomalies or to implant pacemakers. Experts recommend an individualized approach to treating heart conduction disorders, taking into account the characteristics of each clinical case and addressing tactical and strategic tasks to achieve the best long-term outcomes.

Methods for diagnosing heart conduction disorders
Various methods are used to diagnose heart conduction disorders, including electrocardiography (ECG). The ECG allows for the assessment of heart activity, identification of rhythm and conduction abnormalities, as well as determination of changes in the structure of the heart muscle. Additionally, Holter monitoring can be used for prolonged observation of heart activity and detection of arrhythmia episodes.
Modern methods for diagnosing conduction disorders include echocardiography, magnetic resonance imaging, and invasive procedures such as electrophysiological studies. The comprehensive application of these methods allows for a precise determination of the type of heart conduction disorders, their causes, and severity, which is crucial for selecting the optimal treatment strategy and addressing monitoring and prognosis issues.
-
– Electrocardiography (ECG): ECG is the primary method for diagnosing heart conduction disorders. It allows recording the electrical activity of the heart and identifying rhythm and conduction abnormalities.
– Holter monitoring: This method involves continuous ECG recording over an extended period, usually 24 hours or more, to detect periods of arrhythmias that may have been missed during a standard ECG.
– Echocardiography: Echocardiography is used to visualize the structure and function of the heart using ultrasound waves, which helps assess heart function abnormalities and identify issues, including conduction disorders.
– Magnetic Resonance Imaging (MRI): Cardiac MRI provides a detailed image of the heart’s structure and can be used to evaluate conduction disorders in conjunction with other diagnostic methods.
– Invasive methods: Invasive methods include electrophysiological studies that allow examination of the heart’s electrical activity within the heart chamber, which may be necessary for accurately determining the nature of conduction disorders.
Methods for treating heart conduction disorders
Patients with heart conduction disorders may also be prescribed special rehabilitation programs that include physical exercises, diet, and stress management. It is important to individually approach the choice of treatment methods, taking into account the peculiarities of each clinical case, to ensure the most effective management of symptoms and improve the disease prognosis.
- Use of antiarrhythmic drugs: Antiarrhythmic drugs can help restore the normal rhythm of the heart and improve conductivity.
- Pacemaker implantation: For serious conduction disorders, pacemaker implantation may be required to control the heart rate.
- Surgical interventions: In some cases, surgical treatment is necessary to restore normal impulse conduction in the heart.
- Rehabilitation programs: Special rehabilitation programs may include physical exercises, diet, stress management, and other activities to improve the condition of cardiac conductivity.
- Individual approach to treatment: The decision on treatment methods for heart conduction disorders should be individualized, taking into account the characteristics of each patient and their clinical picture, to ensure the most effective management of the disease.
Measures to prevent heart conduction disorders
Conducting regular medical examinations, including ECG and other screening methods, also helps to identify potential heart conduction disorders at early stages and take preventive measures. Patient education about risk factors, adherence to medication prescriptions and doctor’s recommendations, regular monitoring, and maintaining a healthy lifestyle contribute to reducing the likelihood of developing heart conduction disorders and lowering overall cardiovascular risk.
- Maintaining a healthy lifestyle, which includes regular physical activity, a balanced diet, and quitting smoking, contributes to the overall strengthening of the cardiovascular system.
- Monitoring blood pressure and cholesterol levels helps prevent the development of atherosclerosis, which supports the maintenance of normal heart conduction.
- Regular medical examinations, including tests and electrocardiography, allow for the identification of initial changes and conduction disorders in the heart at early stages, enabling timely treatment.
- Avoiding stressful situations, rational alcohol use, and active participation in preventive programs can help reduce the risk of cardiovascular diseases, including conduction disorders.
- Educating and informing patients about risk factors, symptoms, and prevention methods for heart conduction disorders helps prevent diseases and promotes the formation of a healthy lifestyle.
Engaging aspects of heart conduction disturbances
Another interesting fact is that various factors, such as stress, lack of physical activity, poor nutrition, and metabolic disorders, can influence heart conductivity. This aspect highlights the importance of preventive measures and maintaining a healthy lifestyle to prevent the occurrence of heart conductivity disorders.