Trigeminal neuralgia: symptoms, causes, and treatment
- Understanding trigeminal neuralgia
- Destructive causes of trigeminal neuralgia
- The variety of symptoms of trigeminal neuralgia
- Expert view on treatment methods for trigeminal neuralgia
- Approaches to the diagnosis of trigeminal neuralgia
- Innovative methods for treating trigeminal neuralgia
- Measures for the prevention of trigeminal neuralgia
- Amazing aspects of trigeminal neuralgia
- FAQ
Understanding trigeminal neuralgia
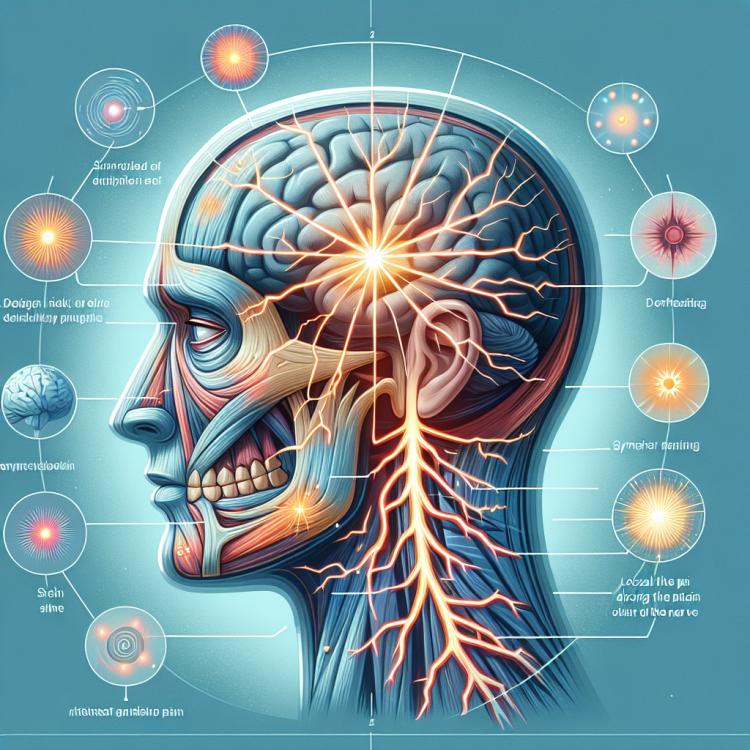
Trigeminal neuralgia, also known as trigeminal neuralgia, is an acute pain that spreads in the facial and head area, caused by irritation of the trigeminal nerve. This type of pain can be intense and paroxysmal, significantly impairing the patient’s quality of life. Understanding trigeminal neuralgia includes knowledge of the structure and function of the trigeminal nerve, common causes of nerve irritation, as well as methods of diagnosis and treatment of this condition, including pharmacological therapy and surgical interventions.
Destructive causes of trigeminal neuralgia
Trigeminal neuralgia, characterized by sharp facial pain, can have many destructive causes. One of the most common is the compression of nerve fibers by blood vessels. Anomalies in the structure of the facial vessels or arteriovenous shunts can lead to pressure on the trigeminal nerve and the onset of pain syndrome. Additionally, trigeminal neuralgia can be caused by inflammatory processes around the nerve or its compression due to tumors in the head and neck area.
- Compression by blood vessels: Anomalies in the structure of the facial vessels can lead to pressure on the trigeminal nerve, causing pain syndrome.
- Inflammatory processes: Inflammation in the facial area or around the trigeminal nerve can lead to irritation and pain.
- Presence of tumors: Tumors in the head or neck area can compress the trigeminal nerve, causing neuralgia.
- Injuries and damage: Mechanical injuries to the face or head can damage the trigeminal nerve, causing pain sensations.
- Neurological diseases: Some neurological diseases, such as multiple sclerosis, may be associated with the development of trigeminal neuralgia.
The variety of symptoms of trigeminal neuralgia
Trigeminal neuralgia is a condition characterized by a variety of symptoms, which can vary depending on the type of neuralgia and the affected area of the face. The main symptom is sharp, stabbing, or shooting pain in the facial area, often occurring in episodes. In trigeminal neuralgia, painful spasms and even loss of sensation in the area innervated by the nerve may also be observed, significantly reducing the patient’s quality of life.
- Sharp pain in the facial area: characterized as stabbing, shooting, or paroxysmal pain, often severely limiting ordinary daily activities.
- Painful spasms: accompanied by intense contractions of the facial muscles, leading to increased pain sensations and discomfort.
- Loss of sensitivity in the innervation zone: there may be partial or complete loss of sensation in the facial area, which deteriorates the patient’s quality of life and can lead to complications while eating or performing other daily activities.
- Pain while chewing or touching the face: often exacerbated by touch to the trigeminal nerve area, such actions can elicit sharp and unpleasant pain.
- Changes in speaking and chewing: due to severe pain and discomfort, patients may experience difficulties while speaking or chewing food, which lowers their overall quality of life.
Expert view on treatment methods for trigeminal neuralgia
Experts’ opinions on the treatment methods for trigeminal neuralgia are based on a comprehensive approach that takes into account the individual characteristics of each patient. One of the key treatment methods for trigeminal neuralgia is medication therapy aimed at reducing pain and lowering inflammation in the surrounding nerve tissues. Experts also emphasize the importance of physiotherapy and rehabilitation procedures in the comprehensive treatment of this condition, such as exercises for the facial muscles, massage, and applications.

Approaches to the diagnosis of trigeminal neuralgia
The diagnosis of trigeminal neuralgia is a complex and multi-stage investigation, including patient history, conducting a neurological examination, and specialized functional tests. A key diagnostic method is often neuroimaging, such as magnetic resonance imaging (MRI) or computed tomography (CT), which allow for the identification of structural changes in the area of the trigeminal nerve and surrounding tissues.
A detailed study of clinical manifestations, as well as the use of modern educational diagnostic methods, helps specialists accurately establish the diagnosis of trigeminal neuralgia and determine the most effective treatment methods for each specific case. It is important to consider the individual characteristics of the patient and to rely on current clinical guidelines to ensure optimal results in the treatment of this condition.
- History and symptoms: An important stage is collecting information about the patient’s medical and family history, as well as identifying the characteristic symptoms of trigeminal neuralgia.
- Neurological examination: Conducting tests of sensitivity, reflexes, motor skills, and other neurological parameters to assess the condition of the trigeminal nerve.
- Functional tests: Utilizing specialized tests, such as pain reaction tests or electrophysiological studies, for additional evaluation of nervous system function.
- Instrumental methods: Applying neuroimaging techniques, including MRI and CT, to visualize the trigeminal nerve and surrounding structures.
- Consultation with specialists: If necessary, it is advisable to consult a neurologist or neurosurgeon for a more in-depth analysis and clarification of the trigeminal neuralgia diagnosis.
Innovative methods for treating trigeminal neuralgia
- Neurostimulation: The use of advanced methods such as deep brain stimulation and transcranial magnetic stimulation to alter the activity of nerve structures and reduce pain in patients with trigeminal neuralgia.
- Pharmacological therapy: The application of innovative pharmacological agents, including anticonvulsants, analgesics, and membrane-stabilizing agents, aimed at reducing pain syndrome in patients.
- Nerve block procedures: The use of modern trigeminal nerve block methods as conservative treatment to reduce pain and improve patients’ quality of life.
- Physical therapy: The application of innovative approaches in physical therapy, such as ultrasound therapy, electrical stimulation, and laser treatment, to reduce pain syndrome and improve the functionality of the trigeminal nerve.
- Surgical methods: The use of advanced surgical techniques, including microvascular decompression and radiofrequency ablation, for the treatment of trigeminal neuralgia in patients for whom more conservative methods are ineffective.
Measures for the prevention of trigeminal neuralgia
- Maintaining a healthy lifestyle: leading an active lifestyle, healthy eating, and giving up bad habits contribute to strengthening the nervous system and overall health of the body.
- Adhering to proper ergonomics in daily activities: the correct posture while using the computer, moderate use of gadgets and communication devices help prevent excessive strain on the neck and face and reduce the risk of developing trigeminal neuralgia.
- Managing stress: regularly practicing relaxation methods, meditation, yoga, or other techniques can help lower stress levels and prevent negative effects on the nervous system.
- Regular medical check-ups: visiting doctors for preventive examinations allows for the identification and timely treatment of possible diseases, preventing complications, including trigeminal neuralgia.
- Avoiding mechanical and chemical irritants: protection from injuries and avoiding contact with irritating substances can help reduce the risk of damage to nerve cell material and the occurrence of trigeminal neuralgia.
Amazing aspects of trigeminal neuralgia
Moreover, a remarkable feature of trigeminal neuralgia is the potential for pain to arise in various areas innervated by the nerve, such as the upper and lower jaws, forehead, cheek, or even the eye socket. Patients may experience pain in different regions of the face and head simultaneously or alternately, which poses a challenge for the medical community in diagnosing and treating this condition.