Uterine prolapse: causes, symptoms, and treatment methods
- Uterine prolapse: understanding the issue
- Factors contributing to uterine prolapse
- Signs and symptoms of uterine prolapse
- Expert opinion on methods for treating uterine prolapse
- Methods for diagnosing uterine prolapse
- Methods of treating uterine prolapse
- Prevention measures for uterine prolapse
- Funny aspects of the uterus removal
- FAQ
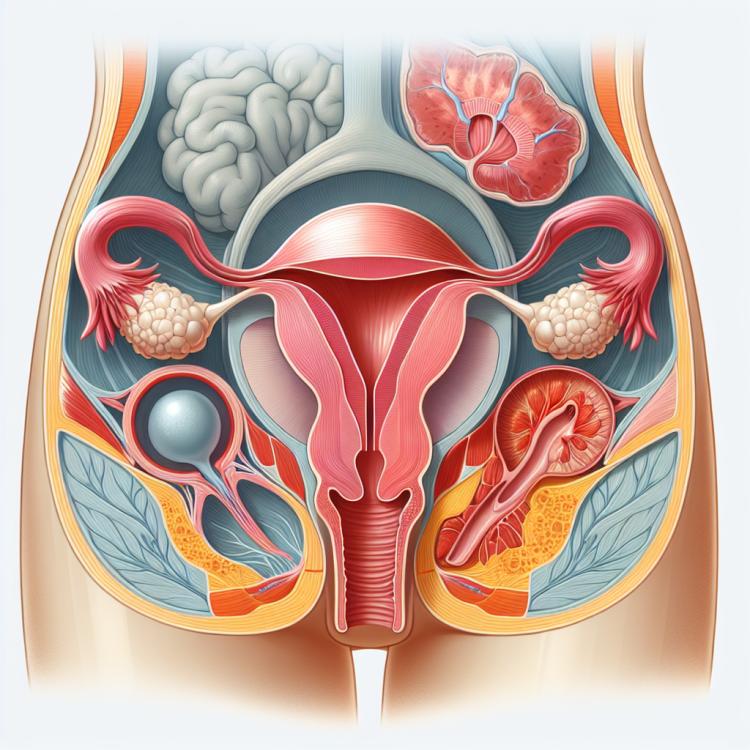
Uterine prolapse: understanding the issue
Uterine prolapse, or uterine ptosis, is a pathological condition in which the uterus shifts from its normal position in the pelvis. This can be caused by weakening of the pelvic floor and ligaments, leading to the descent of the organ into the vaginal cavity. Uterine prolapse is often accompanied by discomfort in the lower abdomen, lower back pain, and may also lead to urinary and sexual dysfunction.
For effective treatment of uterine prolapse, it is important to consult a doctor and undergo appropriate examinations. Treatment may include conservative methods, such as physical therapy and wearing special supportive garments, and in some cases, surgical intervention may be necessary to restore the normal position of the uterus and strengthen its supportive structures.
Factors contributing to uterine prolapse
Uterine prolapse, or uterine ptosis, can be caused by a variety of factors. One of the main reasons is the weakening of the pelvic floor muscles, which are responsible for supporting the pelvic organs, including the uterus. Childbirth, especially delivery using forceps or vacuum extraction, can lead to stretching and weakening of the birth canal, which in turn contributes to uterine prolapse.
Other causes of uterine prolapse may include obesity, smoking, frequent heavy lifting, as well as changes in hormonal balance. Factors that contribute to increased pressure in the abdominal cavity, such as frequent coughing or constipation, can also increase the risk of developing uterine prolapse.
- Weakening of the pelvic floor muscles: A decrease in the tone of the muscles responsible for supporting the uterus can contribute to its prolapse.
- Negative impact of childbirth: Childbirth, especially with the use of obstetric instruments, can lead to stretching of the birth canal and worsen the supportive structures.
- Obesity: Excess weight can increase the pressure in the abdominal cavity, contributing to uterine prolapse.
- Smoking: Tobacco substances can negatively affect the tissues and muscles of the pelvic floor, increasing the risk of uterine prolapse.
- Physical exertion: Excessive lifting of heavy weights or prolonged carrying of heavy objects can increase pressure on the uterus, contributing to its prolapse.
Signs and symptoms of uterine prolapse
Symptoms of uterine prolapse can manifest in various ways, including a feeling of heaviness or pressure in the lower abdomen, especially after prolonged standing or physical exertion. Women with uterine prolapse may also experience pain in the lower abdomen or lower back, as well as discomfort during sexual intercourse. A sensation of “something falling out” of the vagina or visible protrusion of tissue through the vagina may also indicate uterine prolapse.
Other signs and symptoms associated with uterine prolapse may include frequent urination, incontinence, urinary problems, and an increased risk of urinary tract infections. It is important to consult a specialist at the first signs of uterine prolapse for diagnosis and appropriate treatment.
- Feeling of pressure or heaviness in the lower abdomen: a feeling of discomfort or pressure in the pelvic area can be one of the early signs of uterine prolapse.
- Pain in the lower abdomen or lower back: women with uterine prolapse may experience painful sensations in the abdomen or back.
- Discomfort during sexual intercourse: uterine prolapse can lead to painful sensations during sexual intercourse.
- Feeling of “something protruding”: some women may feel protruding tissues through the vagina.
- Frequent urination and incontinence: changes in urination or urinary incontinence may be related to uterine prolapse.
Expert opinion on methods for treating uterine prolapse
Expert opinions on the methods of treating uterine prolapse usually involve an approach tailored to the individual patient’s situation. Experts pay attention to various factors, such as the degree of prolapse, the patient’s age, the presence of comorbidities, and overall health status.
Experts also consider a wide range of treatment methods, including conservative approaches such as physical therapy and the use of pessaries, as well as surgical intervention. A personalized approach and the opinions of experts are important for determining the optimal treatment plan aimed at improving the quality of life for women diagnosed with uterine prolapse.

Methods for diagnosing uterine prolapse
Diagnosis of uterine prolapse usually involves a physical examination by a gynecologist to assess the degree of pelvic organ descent and identify other pathologies. Additional diagnostic methods, such as ultrasound, may be prescribed for a more detailed evaluation of the condition of the uterus, ovaries, and other organs. Sometimes, radiological studies such as urography or cystography may be required to identify concomitant pathologies of the urinary system.
Computed tomography (CT) or magnetic resonance imaging (MRI) may be used for more accurate visualization of the structures of the pelvis and assessment of the degree of prolapse. Accurate diagnosis will help determine an individualized treatment plan, as the effectiveness of the chosen therapy partly depends on the correct identification of the cause and degree of uterine prolapse.
- Physical examination: The gynecologist conducts an external and vaginal examination to determine the degree of uterine prolapse and other changes in the pelvis.
- Ultrasound examination: A method that allows for the visualization of internal organs and evaluation of their condition, including uterine prolapse.
- X-ray examinations: Include urogram and cystography for examining the urinary tract.
- Computed tomography (CT): An examination that uses X-rays to create a three-dimensional image of the pelvic organs.
- Magnetic resonance imaging (MRI): A method that uses magnetic fields for detailed visualization of organs and tissues, including the uterus and ovaries.
Methods of treating uterine prolapse
For moderate and severe degrees of uterine prolapse, surgical intervention may be required, such as vaginal reconstruction or hysterectomy. Surgical methods include various techniques, such as vaginal or abdominal reconstructive surgery, which help return the uterus to its natural position and improve the quality of life for the patient.
- Physical exercises to strengthen the pelvic floor muscles.
- Use of support pads to stabilize the uterus in the correct position.
- Biofeedback and physiotherapy to improve muscle tone.
- Vaginal reconstruction to restore support to the pelvic organs.
- Surgical operations, including hysterectomy, to correct structural defects and restore functions.
Prevention measures for uterine prolapse
An important component of prevention is proper health care, including regular visits to a gynecologist for screening and monitoring the condition of the pelvic organs. Giving birth under the supervision of qualified specialists and timely treatment of any pathologies related to the pelvic organs are also crucial for the prevention of uterine prolapse.
- Regular pelvic floor exercises: Kegel exercises and other exercises aimed at strengthening the pelvic floor muscles help prevent weakening that contributes to pelvic organ prolapse.
- Maintaining a healthy weight: Avoiding excess weight and maintaining a healthy lifestyle help reduce pressure on the pelvic organs and prevent pelvic organ prolapse.
- Avoiding excessive physical strain: Lifting heavy weights or excessive physical exertion can increase the risk of pelvic organ prolapse.
- Proper care for pelvic health: Regular visits to a gynecologist for screening and monitoring the condition of the pelvic organs help identify issues at early stages and prevent pelvic organ prolapse.
- Cautious delivery: Delivery under the supervision of qualified professionals and proper postpartum care are important for preventing pelvic organ prolapse.
Funny aspects of the uterus removal
It is also interesting to realize that with medical attention and proper treatment, uterine prolapse can often be successfully managed, improving the quality of life for patients. This information may encourage women to take care of their health, consult specialists at the first signs, and follow recommendations for their well-being.