Vaginal prolapse: symptoms, causes, and treatment
- Understanding vaginal prolapse
- Main causes of vaginal prolapse
- The main signs of vaginal prolapse
- Expert opinion on the treatment of vaginal prolapse
- Methods for diagnosing vaginal prolapse
- Effective methods for treating vaginal prolapse
- Preventive measures for vaginal prolapse
- Unusual aspects of vaginal prolapse
- FAQ
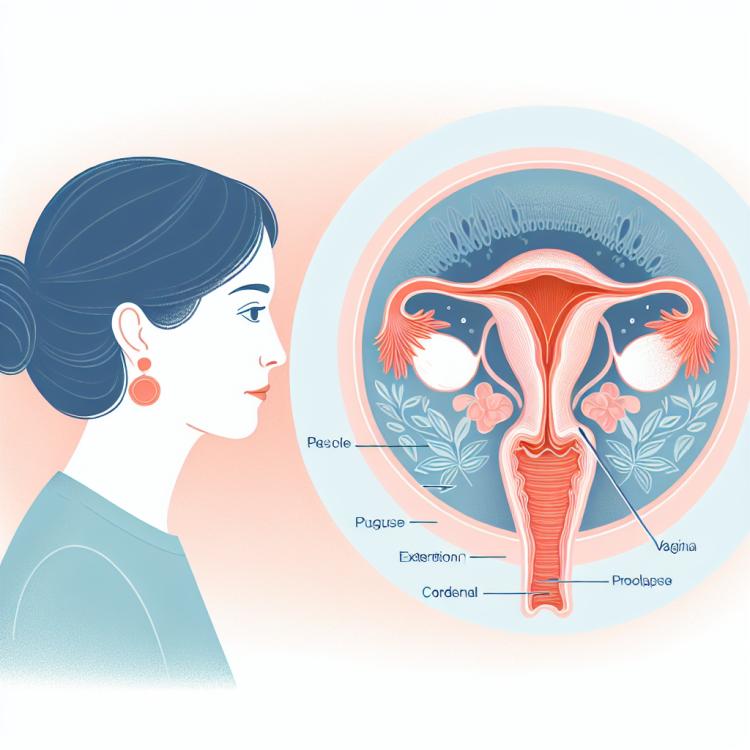
Understanding vaginal prolapse
Vaginal prolapse, or prolapse of the vagina, is a condition characterized by the descent or protrusion of internal structures of the vagina due to weakening of the pelvic floor’s muscular and connective tissue support system. One of the main causes of vaginal prolapse is childbirth, when the tissues of the pelvic floor and ligaments are subjected to significant tension, which can lead to a deterioration of support for the internal organs of the pelvic cavity. Symptoms of vaginal prolapse may include a feeling of pressure or heaviness in the vagina, pelvic pain, as well as discomfort or pain during sexual activity.
It is important to understand that vaginal prolapse can have a negative impact on a woman’s quality of life, causing physical and emotional discomfort. Diagnosis of vaginal prolapse usually includes a physical examination in a gynecological chair and may require the use of additional methods such as ultrasound or MRI. Treatment for vaginal prolapse can be conservative or surgical, depending on the severity of the prolapse and the patient’s desire to maintain or restore the normal anatomy of the pelvic organs.
Main causes of vaginal prolapse
Vaginal prolapse, or perineal-vaginal prolapse, occurs due to weakening of the pelvic floor muscles and ligaments, leading to decreased support for the pelvic organs. The main causes of vaginal prolapse are childbirth tears, surgical interventions in the pelvic area, obesity, chronic heavy lifting, and heredity.
Additionally, factors such as age, the presence of chronic cough, frequent lifting of heavy objects, as well as frequent pregnancies and births, can increase the risk of developing vaginal prolapse. Effective treatment includes strengthening the pelvic floor through special exercises, physiotherapy, and surgical methods in cases where conservative measures have not led to the desired results.
- Childbirth: Giving birth can weaken the pelvic floor muscles and ligaments, increasing the risk of vaginal prolapse.
- Surgical interventions in the pelvic area: Surgeries in the pelvic area can damage tissues and structures, contributing to the development of prolapse.
- Obesity: Excess weight creates additional pressure on the pelvic floor, which can exacerbate vaginal prolapse.
- Chronic heavy lifting: Constant loads and lifting heavy weights can contribute to the stretching and weakening of the pelvic floor muscles.
- Heredity: Genetic factors can influence the structure of tissues and ligaments, increasing the risk of vaginal prolapse.
The main signs of vaginal prolapse
The main symptoms of vaginal prolapse include a feeling of heaviness in the pelvic area, frequent urination, pain or discomfort during sexual intercourse, as well as abnormal vaginal discharge. Women often may experience a sensation of incomplete emptying of the bladder or bowel.
In addition, patients may notice tissue protruding from the vagina or even see it after prolonged standing or straining. It is important to consult a doctor when these symptoms appear, as early seeking of help and proper treatment can prevent complications and improve the quality of life for patients.
- Feeling of heaviness in the pelvic area: women with vaginal prolapse may experience a feeling of pressure or heaviness in the lower abdomen and vagina.
- Frequent urination: sometimes vaginal prolapse can be accompanied by a feeling of needing to constantly empty the bladder.
- Pain or discomfort during intercourse: women may experience painful sensations or discomfort during sexual contact due to the prolapse of vaginal tissues.
- Pathological vaginal discharge: some women with vaginal prolapse may experience changes in the nature of the discharge, such as odor, color, or consistency.
- Feeling of incomplete emptying of the bladder or bowel: patients may feel that they cannot completely empty their bladder or bowel due to compressed vaginal tissues.
Expert opinion on the treatment of vaginal prolapse
Expert opinion on the treatment of vaginal prolapse emphasizes the importance of an individual approach to each patient. Specialized specialists in the fields of gynecology and urology recommend a comprehensive approach that may include conservative methods, such as physical therapy to strengthen the pelvic floor, the use of special elastic devices to support internal organs, as well as surgical intervention in cases where conservative treatment is ineffective.
Experts also highlight the importance of psychological support for patients suffering from vaginal prolapse, as this condition can significantly affect their quality of life. Professional medical consultations and support from specialists help patients understand their treatment options and choose the most suitable path to recovery.

Methods for diagnosing vaginal prolapse
Diagnosis of vaginal prolapse includes a physical examination of the patient, assessing the position of the pelvic organs at rest and during straining. This allows the doctor to determine the degree of prolapse and identify other pathologies that may be associated with this issue. Additionally, an ultrasound examination may be prescribed to evaluate structural changes and the depth of organ prolapse.
Furthermore, other diagnostic methods may be conducted, such as magnetic resonance imaging (MRI) or computed tomography (CT), to obtain a more detailed view of the condition of the tissues and organs in the pelvic area. It is important that the diagnosis is performed by a qualified specialist to accurately identify the causes and choose the optimal treatment plan.
- Physical examination: the doctor evaluates the position of the pelvic organs of the patient at rest and under tension to determine the degree of prolapse.
- Ultrasound examination: allows assessing structural changes and the depth of vaginal organ prolapse.
- Magnetic resonance imaging (MRI): provides detailed images of the organs and tissues in the pelvic area for a more accurate diagnosis.
- Computed tomography (CT): used to obtain a three-dimensional image of the organs and tissues in the pelvic area, allowing the identification of structural changes.
- Transvaginal ultrasound: a special examination that allows a more detailed assessment of the state of the pelvic organs and determines the causes of vaginal prolapse.
Effective methods for treating vaginal prolapse
In cases where conservative methods are not sufficiently effective, surgical intervention should be considered. Surgical methods may include tissue repair and strengthening of support structures to achieve better positioning of the organs and improve the symptoms of vaginal prolapse. It is important to take an individualized approach to the choice of treatment method and discuss all possible options with a qualified specialist.
- Physical therapy and pelvic floor exercises: Exercises aimed at strengthening the pelvic floor muscles can help improve support for the pelvic organs and reduce symptoms of vaginal prolapse.
- Use of vaginal rings or elastic devices: Such devices can help support the vagina and reduce discomfort in cases of prolapse.
- Surgical treatment: In cases where conservative methods do not yield the desired effect, surgical intervention may be necessary to restore supportive structures and the proper position of the vaginal organs.
- Use of medications: In some cases, a doctor may prescribe medications, such as estrogen, to strengthen tissues and improve symptoms of prolapse.
- Lifestyle changes: Adopting a healthy lifestyle, including weight management, moderate physical activity, and preventing chronic muscle tension, can contribute to improving the condition and reducing the risk of vaginal prolapse.
Preventive measures for vaginal prolapse
Additionally, regular check-ups with a gynecologist to identify early symptoms or risks of vaginal prolapse can help take preventive measures. Under the guidance of a specialist, an individual prevention plan can be developed that takes into account the patient’s health features and risk factors.
- Pelvic floor exercises: Regular Kegel exercises help strengthen the pelvic floor muscles and prevent vaginal prolapse.
- Healthy lifestyle: Maintaining a healthy weight, leading an active lifestyle, and proper nutrition contribute to improving the condition of the pelvic tissues and muscles.
- Regular gynecological check-ups: Visiting a doctor for preventive examinations allows for the early detection of problems and timely intervention.
- Avoiding excessive strain: Lifting heavy objects, frequent straining, or prolonged standing can increase the risk of developing vaginal prolapse.
- Individual prevention plan: Developing a unique prevention plan for vaginal prolapse under the guidance of a specialist will help take into account the individual health characteristics of each woman.
Unusual aspects of vaginal prolapse
Another interesting factor is the impact of pelvic organ prolapse on women’s psychological well-being. Often, this dysfunctional symptom can cause feelings of shame, depression, and decreased self-esteem in patients, highlighting the importance of a comprehensive approach to treatment that includes not only physical but also emotional aspects of the condition.