Osteodystrophies: symptoms, causes, and treatment
- Osteodystrophies: concept, essence, and features
- Etiology of Osteodystrophy
- Clinical picture of Osteodystrophy
- Approaches to the treatment of Osteodystrophy: specialists’ viewpoints
- Diagnosis of Osteodystrophy
- Approaches to the treatment of Osteodystrophy
- Prevention of Osteodystrophy
- Interesting aspects of ‘Osteodystrophy’
- FAQ
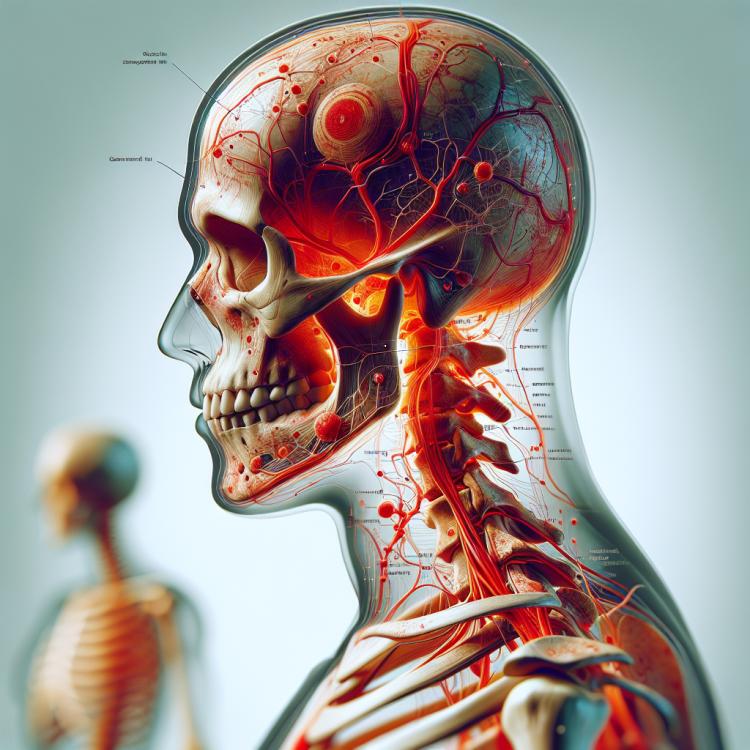
Osteodystrophies: concept, essence, and features
Osteodystrophies are a group of rare, hereditary or acquired diseases of bone tissue. They are based on a disruption of bone formation and healing processes, leading to a deterioration in their structure and function. Osteodystrophies can manifest in various ways, including bone deformities, osteoporosis, osteosclerosis, and other changes that can severely limit patients’ quality of life.
Studying the essence of osteodystrophies is important for developing effective diagnostic and treatment methods. Scientific research reveals the genetic and physiological aspects of these diseases, opening new perspectives for patient treatment. Understanding the features of osteodystrophies allows for the development of individualized approaches for each case, increasing the effectiveness of therapy and improving the prognosis for patients.
Etiology of Osteodystrophy
Osteodystrophy is the result of various factors, including metabolic disorders, nutrient deficiencies, hormonal imbalances, and genetic inheritance. Insufficient intake of calcium and vitamin D in the diet, diseases of the digestive system, as well as endocrine disorders can contribute to the development of osteodystrophy. An important factor is also the lack of physical activity, which can lead to weakening of bone tissue and deterioration of bone structure.
- Imbalance of nutrients: A deficiency of calcium and vitamin D can lead to disorders in the structure of bones.
- Hormonal disorders: Changes in hormone levels, such as parathyroid hormone and calcium, can affect the metabolism of bone tissue.
- Genetic inheritance: Some forms of osteodystrophy may be caused by genetic mutations that are inherited.
- Digestive system diseases: Disorders such as malabsorption can hinder the normal absorption of nutrients necessary for bone health.
- Insufficient physical activity: Lack of regular exercise can lead to weakening of bone tissue and the development of osteodystrophy.
Clinical picture of Osteodystrophy
The clinical picture of osteodystrophy may include various symptoms, such as bone pain, mainly at night or occurring during physical exertion, as well as increased bone fragility. Patients with osteodystrophy may experience limitations in mobility due to pain or weakened bones, which leads to an increased risk of fractures.
The features of the clinical picture of osteodystrophy may vary depending on the type and degree of the disease. Diagnosis is based on the collected medical history, results of physical examination, and instrumental methods of investigation, which allows for a comprehensive picture of the disease to be developed and to determine the optimal treatment plan for each individual patient.
- Bones pain that may worsen with physical activity and be particularly pronounced at night.
- Increased fragility of bones, which may lead to frequent fractures and complications.
- Mobility limitations due to pain and risk of fractures, especially when performing daily activities.
- Deformations of bones or changes in their structure, which may be visible during a physical examination.
- Weakness and swelling in the area of bones that bear greater load, such as the legs and spine.
Approaches to the treatment of Osteodystrophy: specialists’ viewpoints
Experts in the field of rheumatology and orthopedics recommend a comprehensive approach to the treatment of osteodystrophy, including medication therapy, physical rehabilitation, diet, and, in some cases, surgical intervention. Treatment is aimed at reducing pain, restoring bone mass, strengthening bones, as well as preventing fractures and complications related to the disease.
New research in the field of medicine allows for the development of individual treatment plans that take into account the characteristics of each patient. Some specialists also emphasize the importance of lifestyle, physical activity, and proper nutrition in the prevention and treatment of osteodystrophy. The focus on early detection and a comprehensive approach to treatment contributes to improving the quality of life for patients with this condition.

Diagnosis of Osteodystrophy
Diagnosis of osteodystrophy usually involves a comprehensive approach, starting with gathering the patient’s history and physical examination, and ending with instrumental and laboratory studies. Radiological examination can reveal changes in the structure of bone tissue, such as pathological fractures, osteoporosis, as well as signs of osteodystrophy.
Additional diagnostic methods, such as CT, MRI, and bone scintigraphy, may be used for a more detailed study of the condition of bone tissue. Laboratory tests, such as the levels of calcium and vitamin D in the blood, and analysis of bone metabolism markers, can provide information about the overall condition of the bones and assist in the diagnosis of osteodystrophy. A comprehensive approach to diagnosis allows for the determination of the type and degree of the disease, which in turn provides a basis for choosing the optimal treatment strategy.
- Physical examination: The doctor conducts an examination and palpation to identify bone tenderness, limited mobility, and other signs related to osteodystrophy.
- X-ray: Radiological examination allows visualization of bone structure and detection of possible signs of osteodystrophy, such as osteoporosis and fractures.
- Computed tomography (CT) and magnetic resonance imaging (MRI): Additional imaging methods that can provide more detailed information about the condition of bone tissue and allow early-stage changes of osteodystrophy to be seen.
- Bone scintigraphy: An examination that uses radioactive substances to assess the metabolic activity of bone tissue and detect various bone diseases, including osteodystrophy.
- Blood test: Laboratory studies, including measuring levels of calcium, phosphorus, vitamin D, and bone tissue metabolism markers, which can assist in diagnosing osteodystrophy and evaluating the patient’s condition.
Approaches to the treatment of Osteodystrophy
The main goals of osteodystrophy treatment include restoring bone tissue, strengthening bones, reducing pain, preventing fractures, and improving the overall condition of the patient. Patients are provided with individually tailored treatment regimens that take into account their medical history, in order to achieve the best results and prevent possible complications.
- Pharmacological therapy: Includes the use of medications aimed at strengthening bone tissue, improving metabolism, and reducing pain syndrome.
- Physiotherapy: Physical exercises and procedures can help strengthen muscles and bones, increase mobility, and improve the patient’s quality of life.
- Diet therapy: Proper nutrition, rich in calcium, vitamin D, and other nutrients, plays an important role in the treatment of osteodystrophy.
- Surgical methods: In case of complications such as fractures or bone deformities, surgical intervention may be required.
- Preventive measures: Adhering to a healthy lifestyle, moderate physical activity, and regular check-ups with a doctor can help prevent the progression of osteodystrophy.
Prevention of Osteodystrophy
Regular medical examinations aimed at early detection and monitoring the risk of developing osteodystrophy are also important. Education and awareness about risk factors and preventive measures contribute to increasing awareness of osteodystrophy among the population and help to prevent its occurrence.
- A diet rich in calcium and vitamin D helps strengthen bone tissue.
- Regular physical exercises, such as running, swimming, or weightlifting, improve the condition of bones and muscles.
- Avoiding smoking and alcohol consumption helps reduce the risk of developing osteodystrophy.
- Regular medical check-ups and screening studies help identify and monitor the risk of the disease.
- Educating the population about risk factors and the prevention of osteodystrophy contributes to increased awareness and reduced incidence of the disease.
Interesting aspects of ‘Osteodystrophy’
The influence of psychosocial factors on the course of osteodystrophy is also interesting. Stress, depression, and social isolation can negatively affect the progression of the disease and the quality of life of patients. Studies on the relationship between mental health and osteodystrophy help to approach treatment comprehensively and improve the outcomes of examinations for patients with this disease.