Osteophytes: causes, diagnosis, and treatment methods
- Understanding Osteophytes: Essence and Origin
- Pathogenesis of Osteophytes
- The clinical picture of osteophytes
- Expert opinion on the treatment of osteophytes
- Methods of diagnosing osteophytes
- Methods for treating osteophytes
- Measures for the prevention of osteophytes
- Funny facts about osteophytes
- FAQ
Understanding Osteophytes: Essence and Origin
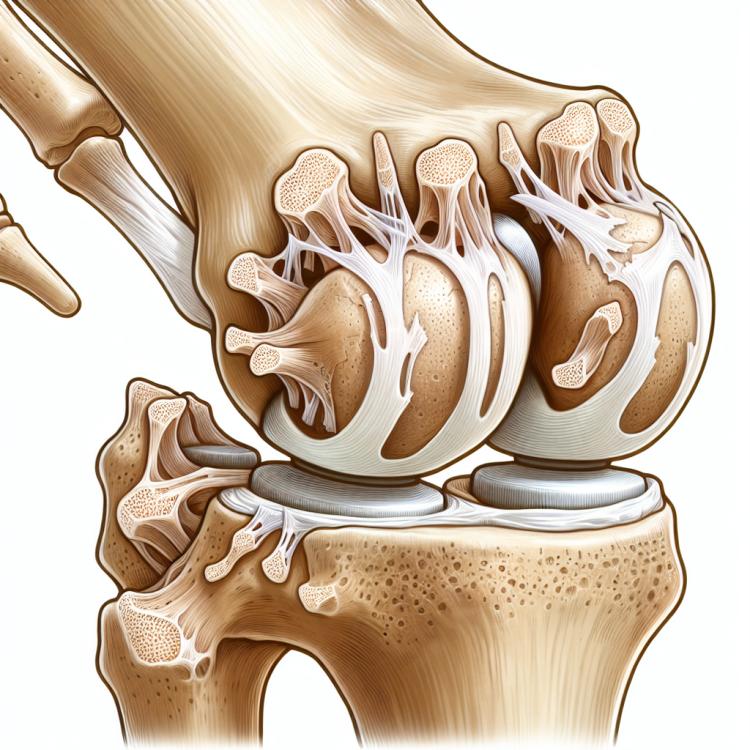
Osteophytes are bone growths that can form as a result of a chronic degenerative process in the joints or spine. The origin of osteophytes is often associated with osteoarthritis—a disease characterized by the destruction of cartilage tissue and joint degeneration. As osteoarthritis develops, new bone tissue grows around the damaged joints, leading to the formation of osteophytes.
These bone growths can cause pain, limit joint mobility, and lead to other symptoms related to adjacent tissues. Understanding the nature and origin of osteophytes is important for determining treatment and prevention strategies for this process, as timely consultation with a doctor can help manage symptoms and prevent complications.
Pathogenesis of Osteophytes
Osteophytes, also known as bone spurs, are projections of bone tissue that form as a result of its growth around joints. The pathogenesis of osteophytes is associated with chronic processes in the joints, such as osteoarthritis or other degenerative diseases. In the case of degenerative changes in the articular cartilage, there is a reactive growth of bone tissue in the areas of damage, which is an attempt by the body to stabilize the joint and restore its function. The presence of osteophytes is often accompanied by degeneration of the joints, which can lead to painful symptoms and impaired mobility.
- Chronic degenerative joint diseases: osteophytes can occur in response to degenerative changes in the articular cartilage typical of various forms of osteoarthritis.
- Mechanical stress: repetitive injuries or improper loading on the joints can contribute to the formation of osteophytes.
- Developmental anomalies of the joints: some congenital or acquired anomalies in the structure of the joints can predispose to the formation of osteophytes.
- Age-related changes: with age, joint tissues are subject to natural wear and tear, which can contribute to the formation of osteophytes.
- Inflammatory processes: chronic inflammation in the joints can stimulate bone tissue growth, leading to the formation of osteophytes.
The clinical picture of osteophytes
The clinical picture of osteophytes may include pain in the area of the affected joint during movement, as well as limited mobility in the joint. The appearance of osteophytes can cause discomfort and inflammation of surrounding tissues, leading to increased pain when bending or straightening the joint.
Other symptoms of osteophytes may include swelling in the joint area, creaking sounds during movement, as well as the appearance of specific protrusions on the skin above the sites of osteophyte formation. The clinical manifestation of osteophytes depends on their size, location, and associated degenerative changes in the joint.
- Pain and discomfort: Patients often complain of joint pain during movement, caused by the rubbing of osteophytes against surrounding tissue.
- Limited mobility: The buildup of bony growths around the joints can lead to restricted mobility and reduced joint function.
- Inflammation and swelling: The formation of osteophytes can trigger inflammatory processes around the joints, accompanied by swelling and redness of the skin.
- Cracking sounds: Sometimes, when moving joints with osteophytes, specific sounds—cracking or crunching—can occur, which may be noticed by the patient.
- Protrusions on the skin: Some patients report the appearance of small protrusions or lumps on the skin above the site of osteophyte manifestation, which may be related to their external appearance.
Expert opinion on the treatment of osteophytes
Expert opinion on the treatment of osteophytes is based on a comprehensive approach that includes conservative and surgical methods. Specialists recommend starting with conservative treatment, such as physiotherapy, medication therapy, physical activity, and a diet aimed at reducing inflammation and pain symptoms.
In cases where conservative treatment does not provide sufficient improvement or when osteophytes lead to serious mobility restrictions in the joint, surgical intervention may be necessary. Expert opinion emphasizes the importance of an individualized approach to selecting the method of treating osteophytes, taking into account the characteristics of each patient and the nature of the disease manifestations.

Methods of diagnosing osteophytes
The diagnosis of osteophytes includes various examination methods, such as radiography, computed tomography (CT), and magnetic resonance imaging (MRI). Radiological examination, such as joint X-rays, allows visualization of bone growths and assessment of their size and the degree of degenerative changes in the surrounding tissues. CT and MRI provide more detailed information about the structure of the joints, which aids in determining the exact location of osteophytes and their impact on surrounding tissues.
An additional method for diagnosing osteophytes may be ultrasound examination, which also allows visualization of the affected areas of the joints and determining the size and shape of the osteophytes. Clinical manifestations of osteophyte symptoms can also be used in the diagnostic process, complementing the results of instrumental studies to establish an accurate diagnosis and plan treatment.
- X-ray: X-ray is a widely used method for diagnosing osteophytes, allowing the visualization of bone growths and assessment of their characteristics.
- Computed Tomography (CT): CT provides a more detailed image of bone structures and osteophytes, which helps in accurately localizing and assessing the size of the changes.
- Magnetic Resonance Imaging (MRI): MRI allows for high-quality imaging of joints and surrounding tissues, which is useful in diagnosing osteophytes.
- Ultrasound examination: Ultrasound can be used to visualize affected areas of the joints, determine changes, and the shape of osteophytes.
- Clinical examination: Examination and assessment of the symptoms of osteophytes, taking into account the patient’s history and physical status, can serve as additional diagnostic methods.
Methods for treating osteophytes
In some cases, if conservative methods do not bring improvement, surgical intervention may be required. Surgical methods for treating osteophytes include the removal of growths, arthroplasty, or arthrodesis, which can improve joint function and relieve pressure on surrounding tissues, reducing pain and inflammation.
- Use of anti-inflammatory medications: Drug therapy often includes the intake of non-steroidal anti-inflammatory drugs to reduce inflammation and pain in the affected joints.
- Physical therapy: Physical therapy procedures, such as ultrasound therapy and laser treatment, help improve blood circulation, reduce inflammation, and relax muscles to alleviate pain symptoms.
- Exercises to strengthen muscles: Systematic exercises to improve the strength and flexibility of the muscles around the joints can reduce the load on the joints and improve their function.
- Injections into the affected joint area: Injections of glucocorticoids or hyaluronic acid directly into the joints can provide relief from pain and inflammation.
- Surgical intervention: If conservative methods yield no results, surgical removal of osteophytes may be required to improve symptoms and restore joint function.
Measures for the prevention of osteophytes
In addition, it is important to avoid injuries and overloads of the joints, and to properly address any professional deformities and diseases that may provoke the development of osteophytes. Regular medical check-ups and timely treatment of joint diseases also contribute to the prevention of osteophyte development.
- Regular physical exercises: Strengthening muscles and maintaining joint flexibility help prevent excessive pressure on joint surfaces.
- Weight control: Maintaining a healthy weight is important as obesity can increase the load on joints and contribute to the development of osteophytes.
- Avoiding injuries and joint overloads: Preventing injuries and avoiding excessive stress on joints will help prevent the development of degenerative changes and the formation of osteophytes.
- Addressing occupational deformities: Correcting occupational deformities and diseases that can provoke the development of osteophytes plays an important role in their prevention.
- Regular medical check-ups and timely treatment: Regular medical monitoring and timely treatment of joint diseases contribute to the prevention of osteophyte development.
Funny facts about osteophytes
Another amusing fact about osteophytes is their variety of shapes and sizes. Osteophytes can be just small projections of bone tissue, but they can also be of more significant sizes and take the form of spurs, sharp projections, or flat growths. This diversity in the shape of osteophytes makes them unique objects of study in medical practice.