Osteochondrosis of the cervical spine: symptoms, causes, and treatment methods
- Understanding Cervical Osteochondrosis
- Factors contributing to the development of cervical osteochondrosis
- The main symptoms of cervical osteochondrosis
- Expert opinions on the treatment of cervical spine osteochondrosis
- Methods of diagnosing cervical spine osteochondrosis
- Methods of treating cervical osteochondrosis
- Measures for the prevention of cervical osteochondrosis
- Interesting aspects of cervical spine osteochondrosis
- FAQ
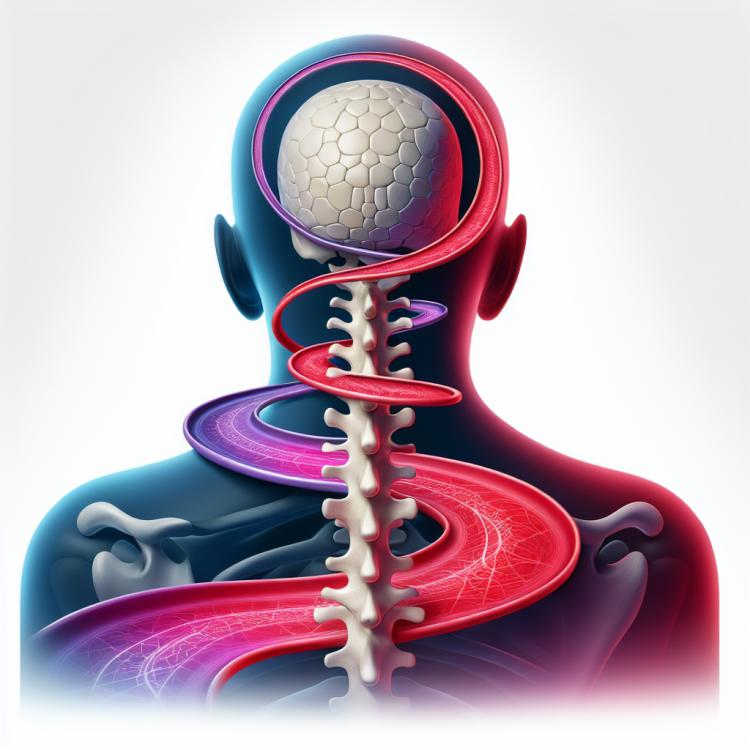
Understanding Cervical Osteochondrosis
Cervical osteochondrosis is a degenerative disease characterized by damage to the intervertebral discs, facet joints, and soft tissues of the cervical spine. This disease is marked by disruption of the structure and function of the intervertebral discs, leading to various clinical manifestations such as neck pain, headaches, and sensations of numbness and weakness in the arms.
Understanding the main causes and mechanisms of cervical osteochondrosis development is important for accurate diagnosis and effective treatment. Unhealthy diet, sedentary lifestyle, excessive strain on the cervical spine, age-related changes, and genetic predisposition can contribute to the development of this disease. In addition to conservative treatment, surgical intervention may be required in some cases to address the consequences of cervical osteochondrosis.
Factors contributing to the development of cervical osteochondrosis
The formation of cervical osteochondrosis can be caused by a variety of factors, including a sedentary lifestyle, increased stress on the neck due to computer work or prolonged reading, as well as traumatic injuries that can lead to degenerative changes in the cervical spine. Postural disorders and spinal deformations can also contribute to the development of cervical osteochondrosis by increasing the load on intervertebral discs and neck structures.
In addition, age-related changes, metabolic disorders, and genetic predisposition can also play a role in the formation of cervical osteochondrosis. Maintaining a healthy lifestyle, regular exercises to strengthen the back and neck muscles, as well as proper posture while performing daily tasks can help reduce the risk of developing this condition.
- Sedentary lifestyle: prolonged sitting at a computer or behind the wheel can lead to weakened neck muscles and decreased mobility of the spine.
- Increased tension on the neck: constant tilting of the head while working at a computer or reading can put additional pressure on the cervical spine.
- Traumatic injuries: wounds, bruises, or other injuries to the neck can lead to the development of degenerative changes and osteochondrosis.
- Posture disorders: improper body position or scoliosis can create additional strain on the cervical spine.
- Age and hereditary factors: aging of the body, as well as genetic predisposition, can contribute to the development of cervical osteochondrosis.
The main symptoms of cervical osteochondrosis
The main symptoms of cervical osteochondrosis are pain in the neck and shoulders, which may worsen when turning the head or bending it. This pain can also radiate to the head, arms, and upper limbs. Patients may also experience a sensation of numbness, tingling, or weakness in the neck, shoulders, and arms.
Other typical symptoms of cervical osteochondrosis may include ringing in the ears, a feeling of dizziness, reduced skin sensitivity in the neck area, and limited neck mobility. It is important to follow preventive measures aimed at strengthening the neck muscles, and in case of the above-mentioned symptoms, to seek consultation with a doctor for diagnosis and appropriate treatment.
- Pain in the neck and shoulders: often worsens with movements of the head and arms, and may radiate to the upper limbs.
- Numbness and tingling: occur in the neck, shoulders, and arms due to pressure on the nerve structures.
- Restricted neck mobility: patients feel stiffness and difficulties when turning their heads.
- Sensation of dizziness: may occur with increased strain on the cervical spine.
- Tinnitus and changes in skin sensitivity: may also accompany cervical osteochondrosis.
Expert opinions on the treatment of cervical spine osteochondrosis
Experts in the field of medicine attribute effective treatment of cervical osteochondrosis to a comprehensive approach. First and foremost, the focus is on managing pain and inflammation through the use of medications, physiotherapy, and exercises aimed at strengthening the cervical spine and reducing strain on the discs. Additionally, orthopedic specialists and rehabilitation professionals recommend an individualized treatment approach, taking into account the specific characteristics of the disease in each patient.
Experts also emphasize the importance of preventing exacerbations and the long-term effects of treatment. Special attention is given to the patient’s lifestyle, correcting bad habits, maintaining proper posture while performing daily tasks, and following recommendations for spinal care. Successful treatment of cervical osteochondrosis not only reduces pain and improves quality of life but also helps prevent potential complications and maintain the functionality of the cervical spine in the long term.

Methods of diagnosing cervical spine osteochondrosis
The diagnosis of cervical spine osteochondrosis usually begins with a medical examination and a conversation with the patient to identify characteristic symptoms and the history of the disease. To confirm the diagnosis and assess the condition of the spine, various instrumental methods may be used, including X-ray, magnetic resonance imaging (MRI), or computed tomography (CT). These methods allow doctors to see changes in the structure of the spine, assess the degree of damage to the intervertebral discs, and identify other pathologies that may accompany osteochondrosis.
In addition to instrumental studies, specialists may conduct additional tests, such as a neurological examination, to assess the function of the nervous system and determine the extent of nerve root involvement. A comprehensive approach to diagnostic procedures allows for the identification of the degree of development of cervical spine osteochondrosis and the planning of effective treatment on an individual basis.
- Medical examination and history: The doctor conducts an examination, discussing characteristic symptoms and the history of the disease to begin the diagnosis of cervical osteochondrosis.
- X-ray: X-ray images allow for the visualization of the structure of the spine and the identification of degenerative changes in the cervical region.
- Magnetic Resonance Imaging (MRI): This method provides more detailed images of the spine, detects disc herniations, and evaluates the condition of soft tissues.
- Computed Tomography (CT): CT helps identify detailed anatomical information about the condition of the spine and intervertebral discs.
- Neurological examination: The doctor checks the function of the nervous system, reflexes, and sensitivity to assess the involvement of nerve structures in the pathological process.
Methods of treating cervical osteochondrosis
In cases of cervical spine osteochondrosis where conservative methods do not provide adequate relief, injection treatment methods may be used, such as blockades, administration of anti-inflammatory drugs, or analgesics. In some instances, when the progression of the disease leads to severe pain or deformities, surgical intervention may be considered to restore the normal structure of the spine and reduce compression on nerve structures. Treatment of cervical spine osteochondrosis should be individualized and based on consultation with an experienced specialist.
- Physiotherapy: Includes exercises to strengthen the back and neck muscles, massage, as well as procedures to improve blood circulation in the spinal area.
- Injection treatment methods: Include blocks, the introduction of anti-inflammatory drugs or those providing analgesia.
- Non-drug treatment: Physical therapy, massage, alternative methods such as yoga or Pilates, as well as maintaining good posture in daily life.
- Surgical intervention: A treatment method that may be considered in cases where disease progression leads to severe pain, deformities, or compression of nerve structures.
- Individualized approach: Treatment of cervical osteochondrosis should be based on consultation with an experienced physician and calculated according to the individual characteristics of the patient and the stage of disease development.
Measures for the prevention of cervical osteochondrosis
In addition, it is important to properly organize the workspace, ensuring ergonomic conditions for working at the computer, as well as to take regular breaks and perform stretching exercises. Adhering to a healthy lifestyle, including a diet rich in vitamins and minerals, avoiding harmful habits, maintaining an optimal weight, and monitoring posture, contributes to the prevention of cervical osteochondrosis and the overall health of the spine.
- Regular physical exercise: engaging in moderate physical activities aimed at strengthening the muscles of the back and neck helps reduce the risk of developing cervical osteochondrosis and supports the overall health of the spine.
- Correct posture: attention should be paid to the proper body position when sitting, standing, and walking, which promotes even weight distribution on the spine and prevents deformities.
- Organization of the workplace: it is important to ensure ergonomic conditions in the office or at home by using a comfortable chair, a footrest, and the correct desk height, which will reduce negative impacts on the spine throughout the day.
- Proper nutrition: the diet should be balanced and contain sufficient vitamins and minerals necessary for the health of bones and cartilage, contributing to the strengthening of the spine.
- Weight control and healthy lifestyle: maintaining a normal weight, avoiding harmful habits, regular medical check-ups, and an active lifestyle contribute to overall health and the strengthening of the spine.
Interesting aspects of cervical spine osteochondrosis
Another interesting aspect of cervical spine osteochondrosis is its impact on the quality of life and productivity of patients. Neck pain and limited mobility can significantly impair professional activities and daily life, emphasizing the importance of timely detection and treatment of this condition to prevent long-term negative consequences.