Osteomyelitis: symptoms, causes, and the latest treatment methods
- Understanding Osteomyelitis: Symptoms, Causes, Treatment, Prevention
- Risks of developing osteomyelitis
- How does osteomyelitis manifest?
- Expert opinions on the treatment of osteomyelitis
- Methods of diagnosing osteomyelitis
- Methods of treating osteomyelitis
- Measures for the prevention of osteomyelitis
- Facts about osteomyelitis
- FAQ
Understanding Osteomyelitis: Symptoms, Causes, Treatment, Prevention
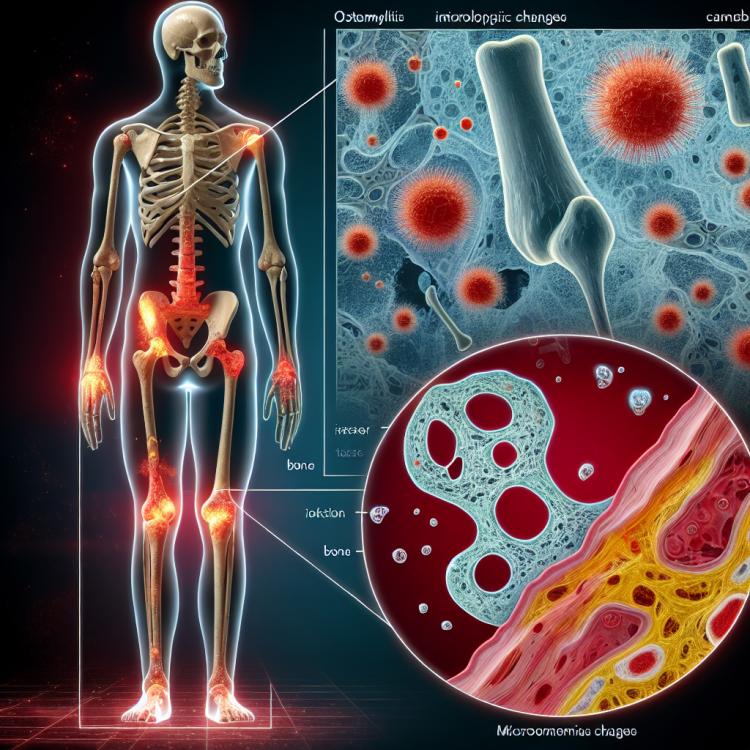
Osteomyelitis is a serious infectious disease of the bones, characterized by inflammation and destruction of bone tissue. Symptoms of osteomyelitis may include high fever, pain in the affected bone area, swelling, and redness of the skin. The cause of osteomyelitis is most often bacterial infections that penetrate the bone through a wound or bloodstream, making early diagnosis and appropriate treatment necessary to prevent complications.
Treatment of osteomyelitis typically includes the use of antibiotics to combat the infection, and in some cases, surgical intervention may be required to remove necrotic tissue. Prevention of osteomyelitis includes adhering to hygiene rules when dealing with wounds, timely treatment of infections, and strengthening immunity to prevent the possibility of developing this serious disease.
Risks of developing osteomyelitis
Osteomyelitis is a serious infectious disease caused by bacteria that penetrate the bone through trauma, surgical intervention, or bloodstream. The risks of developing osteomyelitis are significantly increased in individuals with impaired blood supply to the bones, diabetes, reduced immunity, as well as in patients with prosthetics or drainage systems.
There are also factors that increase the likelihood of developing osteomyelitis, such as nutrient deficiencies, prolonged use of steroids or chemotherapy, the presence of chronic wounds or ulcers, and certain hereditary diseases. Preventing osteomyelitis involves timely treatment of infections, proper care of wounds and injuries, as well as managing factors that contribute to reduced blood supply to the bones or suppression of the immune system.
- Circulation disorders: Impaired circulation increases the risk of osteomyelitis due to weakened immune cell ability to fight infection.
- Diabetes mellitus: Patients with diabetes mellitus are at high risk of developing osteomyelitis due to metabolic disorders and decreased immune protection.
- Immunodeficiency: Reduced immunity makes the body vulnerable to bacteria, increasing the likelihood of bone tissue infection.
- Prosthetics: The presence of orthopedic implants increases the risk of bone infection by bacteria and the development of osteomyelitis.
- Chronic wounds: The presence of long-lasting wounds or ulcers on the skin is also a risk factor, as they can provide pathways for infection to enter the body.
How does osteomyelitis manifest?
Osteomyelitis manifests with a variety of symptoms, including pain in the affected bone or joint, swelling and redness of the skin around the affected area, general weakness, fever, and increased sweating. Patients may also experience a sensation of warmth in the area of the affected bone, limited mobility in the joint, and sometimes even pus from the wound or the presence of pustules on the skin.
Some forms of osteomyelitis may present more subtly, especially in elderly individuals or patients with weakened immune systems. Suspicions of osteomyelitis may arise with persistent pain in the bone area that does not respond to standard pain treatment or antibiotics, highlighting the importance of consulting a doctor for the diagnosis and treatment of this serious condition.
- Pain and swelling: Osteomyelitis is often accompanied by intense pain in the affected bone or joint, which worsens with movement. Swelling and redness of the skin around the affected area may also be noticeable.
- General weakness and elevated body temperature: Patients with osteomyelitis may experience general weakness, fatigue, increased sweating, and fever, indicating the presence of infection in the body.
- Sensation of warmth in the area of the affected bone: Some patients may feel increased temperature or warmth in the area of the affected bone, which may indicate an inflammatory process.
- Limited mobility in the joint: In cases of joint involvement with osteomyelitis, patients may experience limited mobility, pain when bending or straightening the joint.
- Presence of pustules on the skin: In some cases, osteomyelitis may manifest as pustules, rashes, or suppurations on the skin, indicating the presence of infection in the tissues.
Expert opinions on the treatment of osteomyelitis
Experts in orthopedics and infectious diseases express a unanimous opinion on the importance of timely diagnosis and comprehensive treatment of osteomyelitis. The standard approach to treatment includes the use of antibiotics, surgical intervention to remove infection from the bone or ensure adequate drainage of the purulent focus, if necessary.
Many experts also emphasize the significance of an individualized approach to the treatment of osteomyelitis depending on the type of infection, its location, and the characteristics of the patient. A wide range of modern methods for diagnosis and treatment, including the use of the latest antibiotics, surgical revision, as well as the use of bone grafting techniques, allows for effective removal of the infection and restoration of the function of the affected bone.

Methods of diagnosing osteomyelitis
The diagnosis of osteomyelitis is based on a comprehensive approach, which may include clinical examination, laboratory tests, imaging diagnostics (X-ray, CT, MRI), and sometimes a biopsy of the affected bone. Clinical symptoms such as pain, swelling, and signs of inflammation may indicate a possible presence of osteomyelitis, while laboratory indicators like the level of C-reactive protein and leukocyte count can help assess the degree of inflammation.
Additional imaging diagnostic methods such as X-ray assist in visualizing changes in the affected bone, while more advanced techniques like MRI or CT can help determine the extent of infection and bone damage. Sometimes, a biopsy is required to clarify the diagnosis, where a sample of the affected tissue is taken for laboratory analysis. Proper diagnosis of osteomyelitis is crucial for accurately determining treatment methods and prognosis for the patient.
- Clinical examination: The doctor examines the patient for signs of inflammation and bone damage.
- Laboratory tests: Studying the levels of C-reactive protein and the number of leukocytes helps determine the presence of inflammation and infection.
- X-ray: X-ray images are used to visualize changes in the bones and determine the stage of the disease.
- Computed tomography (CT): Allows for more detailed images of the affected bones and surrounding tissues.
- Magnetic resonance imaging (MRI): Provides information on the extent of infection and bone damage.
Methods of treating osteomyelitis
Additional treatment methods for osteomyelitis may include the use of anti-inflammatory medications to reduce pain and inflammation, as well as supportive procedures to accelerate rehabilitation and recovery of the affected area. Proper and timely treatment of osteomyelitis is very important to prevent complications and preserve the function of the affected bone.
- Antibiotic therapy: A treatment method based on the use of antibiotics to eliminate the causative agent of the infection.
- Surgical intervention: In cases of severe osteomyelitis, surgery may be required, including drainage of purulent foci and cleaning of the affected bone.
- Anti-inflammatory agents: Used to reduce pain and inflammation in the affected area.
- Physiotherapy: Supportive procedures aimed at restoring the function of the affected bone and accelerating the rehabilitation process.
- Treatment of complications: In the case of complications such as pseudoarthroses or recurrent infections, additional treatment methods may be necessary.
Measures for the prevention of osteomyelitis
For patients with circulatory disorders or immune system issues, it is important to take steps to prevent injuries and infections, as this can contribute to the development of osteomyelitis. Education on preventive measures, proper application of antiseptics for wounds, and subsequent monitoring of the condition of wounds will also help reduce the risk of osteomyelitis.
- Proper wound care: it is important to maintain cleanliness and dryness of wounds, monitor their healing, and consult medical professionals at signs of infection.
- Management of chronic diseases: patients with diabetes or other conditions that increase the risk of osteomyelitis should adhere to the treatment plan and regularly consult with a doctor to monitor their condition.
- Avoiding injuries and infections: for patients with immune system disorders, it is crucial to avoid injuries and contact with potential sources of infection to prevent the development of osteomyelitis.
- Education on preventive measures: patients should be informed about methods to prevent infections and the proper use of antiseptics for skin and wound care.
- Regular monitoring of wound condition: it is important to closely observe the healing of wounds after injury or surgery and consult a doctor at signs of inflammation or infection.
Facts about osteomyelitis
It is important to note that some people are more susceptible to the development of osteomyelitis, such as those with immune system disorders, diabetes, or the presence of prosthetics or surgical drains. Osteomyelitis can be difficult to treat due to its chronic nature, so it is crucial to observe all preventive measures and seek help promptly when symptoms of infection in the bone area appear.