Acute glomerulonephritis: symptoms, diagnosis, and treatment
- Understanding Acute Glomerulonephritis
- Provoking factors of Acute glomerulonephritis
- Recognition of symptoms of Acute Glomerulonephritis
- Clarity of experts’ judgment on the treatment of Acute Glomerulonephritis
- Methods for diagnosing Acute Glomerulonephritis
- Therapy of Acute Glomerulonephritis
- Methods of preventing Acute Glomerulonephritis
- Interesting aspects about Acute glomerulonephritis
- FAQ
Understanding Acute Glomerulonephritis
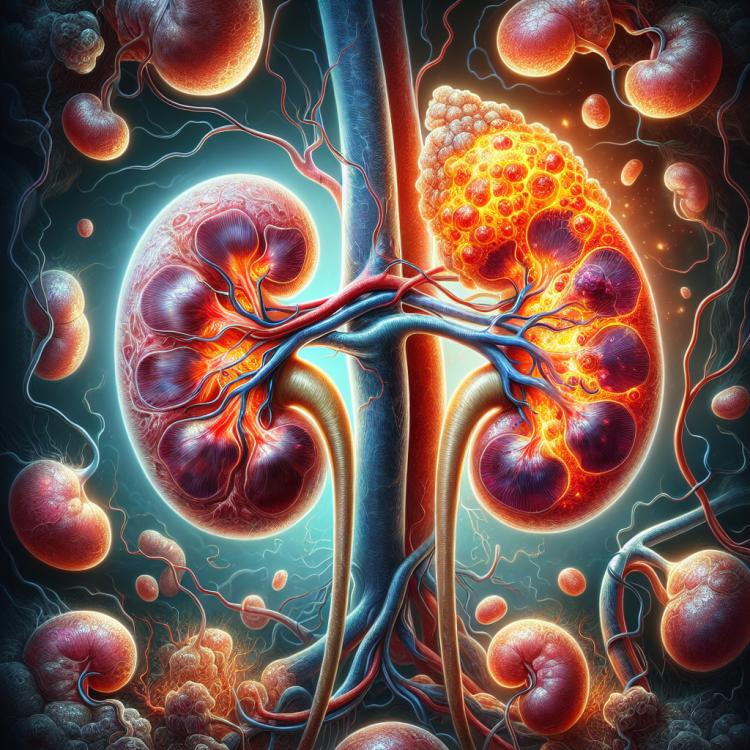
Acute glomerulonephritis is an inflammatory kidney disease characterized by damage to the glomerular apparatus. This disrupts the kidney’s filtration function due to the inflammatory response in the glomeruli, leading to edema, changes in urine, and increased blood pressure. The pathogenesis is based on immune mechanisms, including immune complexes, vascular anomalies, and cellular mediators.
Acute glomerulonephritis can be triggered by infectious agents such as streptococci, as well as autoimmune reactions. Important clinical manifestations include proteinuria, hematuria, azotemia, edema, and hypertension. Timely recognition of symptoms and consulting a doctor for a comprehensive analysis and appropriate therapy is crucial for diagnosis and effective treatment.
Provoking factors of Acute glomerulonephritis
Acute glomerulonephritis, characterized by inflammation of the kidney glomeruli, can be triggered by various provoking factors. One of the main causes of this disease is immunological disorders, where immune complexes deposit in the kidney glomeruli, leading to inflammation. Other causes may include infections, such as staphylococcal or streptococcal infections, as well as systemic diseases like systemic lupus erythematosus or Goodpasture’s syndrome, etc.
In addition, certain medications, such as non-steroidal anti-inflammatory drugs (NSAIDs), antibiotics, or even diuretics, can be factors contributing to the development of acute glomerulonephritis. It is important to identify and eliminate these provoking factors for the successful treatment of this disease and the prevention of its recurrences.
- Immunological disorders: deposition of immune complexes in the renal glomeruli can cause inflammation.
- Infections: staphylococcal or streptococcal infections can be the cause of acute glomerulonephritis.
- Systemic diseases: such as systemic lupus erythematosus or Goodpasture’s disease, can trigger the development of the disease.
- Medications: some drugs, including NSAIDs, antibiotics, and diuretics, can be risk factors for acute glomerulonephritis.
- Genetic factors: hereditary predisposition may also play a role in the development of this disease.
Recognition of symptoms of Acute Glomerulonephritis
Acute glomerulonephritis presents a variety of symptoms, but the most characteristic are edema, most often of the eyelids, limbs, and periorbital area, as well as elevated blood pressure. Patients often experience back pain and the presence of blood in the urine. General symptoms such as fatigue, fever, and loss of appetite may also occur. Signs of acute renal failure may also develop, manifesting as increased levels of creatinine and uric acid in the blood.
Diagnosis is based on clinical signs, laboratory tests (including a urine test for the presence of protein and erythrocytes), and instrumental studies such as kidney ultrasound. If acute glomerulonephritis is suspected, timely consultation with a specialist is necessary for diagnosis and appropriate treatment.
- Edema: Most often of the eyelids, legs, and periorbital area.
- Increased blood pressure: One of the characteristic signs of acute glomerulonephritis.
- Lower back pain: May be accompanied by the presence of blood in the urine.
- General symptoms: Include general weakness, fever, and loss of appetite.
- Signs of acute renal failure: Include an increase in creatinine and uric acid levels in the blood.
Clarity of experts’ judgment on the treatment of Acute Glomerulonephritis
The experts’ opinion on the treatment of acute glomerulonephritis is based on a comprehensive approach, which includes the use of anti-inflammatory and immunosuppressive drugs, blood pressure control, a diet with limitations on proteins and salt, as well as recommendations for preserving kidney function. An individualized approach to treatment, depending on clinical manifestations and possible complications, plays an important role in the successful outcome for the patient.
Experts emphasize the importance of regular monitoring of kidney condition and blood pressure control to prevent disease progression and the development of chronic kidney failure. At the same time, it is important to consider the individual characteristics of each patient and take into account the possible side effects of medications when developing a treatment program for acute glomerulonephritis.

Methods for diagnosing Acute Glomerulonephritis
The diagnosis of acute glomerulonephritis includes various methods, such as a urine test for the presence of protein and red blood cells, measurement of blood pressure, as well as examination of the patient for swelling and other characteristic symptoms. However, the main diagnostic method is kidney biopsy, which allows for determining the degree of inflammation and damage to the renal glomeruli and tubules, identifying the nature of tissue damage, and revealing the underlying cause of the disease.
Additional diagnostic methods may include ultrasound examination of the kidneys to assess their size and structure, as well as tests of kidney function through blood and urine analysis. It is important to conduct the diagnosis of acute glomerulonephritis in a timely manner to determine the correct treatment and prevent complications such as chronic renal failure.
- Urinalysis: Conducting a urinalysis to assess the levels of protein and red blood cells, which may indicate the presence of inflammation in the kidneys.
- Blood pressure measurement: A procedure to detect hypertension, a common accompanying symptom of acute glomerulonephritis.
- Examination for edema and other symptoms: A detailed physical examination of the patient to identify characteristic signs of the disease, such as edema and elevated blood pressure.
- Kidney tissue biopsy: An invasive method that allows the assessment of the degree of inflammation and damage to the renal glomeruli and tubules.
- Ultrasound examination of the kidneys: A non-invasive method used to assess the size, structure, and condition of kidney tissues.
Therapy of Acute Glomerulonephritis
In addition, controlling blood pressure, regulating fluid and electrolyte balance, as well as maintaining kidney function are important aspects of the therapy for acute glomerulonephritis. In some cases, additional treatment of complications, such as renal failure, may be necessary. All treatment measures should be carried out under the supervision and guidance of an experienced specialist.
- Use of anti-inflammatory medications: Includes glucocorticoids to suppress the immune response and reduce inflammation in the kidney glomeruli.
- Blood pressure control: To prevent further kidney damage and complications.
- Regulation of fluid and electrolyte balance: Important for maintaining normal kidney function and preventing edema.
- Individualized approach to treatment: Takes into account the characteristics of each patient and specific case to achieve the best results.
- Monitoring kidney function: Regular observation of kidney function to timely identify and manage possible complications and changes.
Methods of preventing Acute Glomerulonephritis
For individuals at increased risk of developing acute glomerulonephritis, such as patients with prior kidney diseases or immunodeficiency, it is important to undergo systematic medical monitoring and follow all physician recommendations for preventing complications. Effective prevention begins with awareness of one’s own health and seeking medical help promptly at the first signs of the disease.
- Maintaining a healthy lifestyle: a proper diet, regular physical activity, and avoidance of harmful habits help strengthen the immune system and reduce the risk of acute glomerulonephritis.
- Observing hygiene measures: regular handwashing, avoiding contact with infectious agents, and proper separation of personal hygiene items can help prevent the development of an infectious process that contributes to acute glomerulonephritis.
- Preventing hypothermia: maintaining a warm body temperature, especially in cold weather, protects the kidneys from possible negative effects, reducing the likelihood of acute inflammation.
- Early consultation with a doctor: upon the first signs of the disease, such as swelling, pain in the kidney area, or changes in urine, it is important to seek medical help in a timely manner for the diagnosis and treatment of acute glomerulonephritis.
- Following the doctor’s recommendations: for patients at increased risk of developing acute glomerulonephritis, it is particularly important to follow all the specialist’s recommendations, undergo regular examinations, and monitor kidney health for timely detection and prevention of complications.
Interesting aspects about Acute glomerulonephritis
Equally interesting is the fact that acute glomerulonephritis can lead to serious complications, such as chronic kidney failure, if not detected and treated in a timely manner. Therefore, it is important to pay attention to the early signs of the disease, such as swelling, changes in urine, and high blood pressure, and to consult a doctor for further diagnosis and treatment. Receiving timely medical assistance and following the recommendations of specialists are crucial steps in preventing complications and successfully treating acute glomerulonephritis.