Retinal Detachment: Diagnosis, Causes, and Treatment
- Understanding retinal detachment: symptoms, causes, and consequences
- Factors contributing to retinal detachment
- Significant signs of retinal detachment
- The experts’ approaches to treating retinal detachment
- Methods for diagnosing retinal detachment
- Effective methods for treating retinal detachment
- Measures to prevent retinal detachment
- Fascinating aspects of retinal detachment
- FAQ
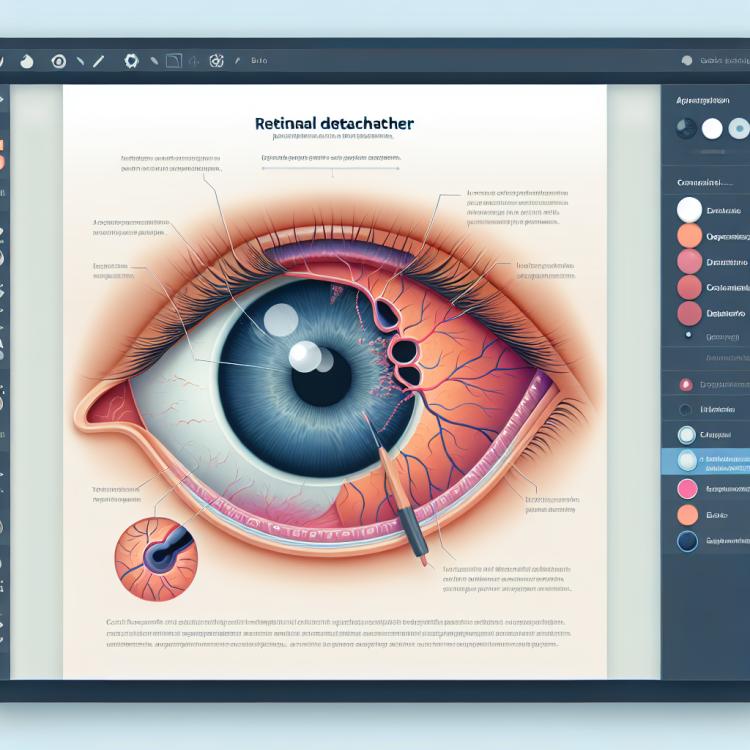
Understanding retinal detachment: symptoms, causes, and consequences
Retinal detachment is a serious eye disease characterized by the separation of the retina from the choroid due to tears or ruptures in the inner layers of the retina. Symptoms of this condition may include vision loss, flash-like bursts of light, floating shadows, or darkening in the field of vision. The cause of retinal detachment is usually the pulling of internal components of the eye, such as diabetic retinopathy, trauma, or age-related changes.
Failure to receive timely treatment for retinal detachment can lead to serious consequences, including complete vision loss in the affected eye. The main goal of treatment is to prevent further retinal detachment by performing surgical intervention, typically through retinal surgery methods aimed at restoring and stabilizing the position of the retina.
Factors contributing to retinal detachment
Retinal detachment can be caused by several factors, including eye trauma, congenital anomalies, or age-related changes. Trauma, especially a blow or strong impact to the eye, can lead to tears in the retina, resulting in its detachment. Congenital anomalies, such as defects in the structure of the eye, can increase the risk of developing retinal detachment. Age-related changes, including age-related degenerative processes, can also be predisposing factors for this condition.
Additionally, individuals with high myopic refraction or a family history of retinal detachment are also at increased risk. Understanding these factors contributing to the development of retinal detachment plays an important role in the diagnosis, prevention, and treatment of this condition.
- Eye injury: Blows, wounds, or other injuries can lead to tears in the retina, causing it to detach.
- Congenital anomalies: Defects in the structure of the eye can increase the likelihood of retinal detachment.
- Age-related changes: As the eyes age, the degenerative process associated with aging may contribute to retinal detachment.
- High myopic refraction: People with high degrees of myopia are at greater risk of retinal detachment.
- Family predisposition: Hereditary factors may also play a role in increasing the likelihood of retinal detachment.
Significant signs of retinal detachment
Retinal detachment may manifest with a number of characteristic symptoms, including the sudden appearance of flashes of light or lightning-like flickers in the field of vision, a reduction or distortion of visual perception, as well as the appearance of darkening in the center of the visual field. Patients may report seeing shadows, as if something is “floating” in front of their eyes, as well as a sense of loss of peripheral vision. In the case of retinal detachment, there is often a sensation of a “curtain” or “veil” obscuring vision.
It is important to note that the symptoms of retinal detachment can gradually intensify over time, so even a slight change in visual sensations requires immediate attention from a specialist for diagnosis and determination of further treatment. Early detection of signs of retinal detachment and timely medical assistance play a crucial role in preventing severe complications and preserving visual function.
- Sudden appearance of flashes of light: a common symptom of retinal detachment, may be accompanied by bursts of light in the field of vision.
- Distortion of visual perception: blurriness, distortions of shapes and colors in the central vision area may indicate potential retinal detachment.
- Visual darkening: the appearance of dark spots or darkening in the center of the field of vision indicates a potential disruption in the structure of the retina.
- Sensation of a curtain in front of the eyes: perception of a “curtain” or “veil” obstructing the view may be a sign of significant retinal detachment.
- Periodic visibility of shadows: perception of shadows as if something is “floating” in front of the eyes may indicate a problem with the retina.
The experts’ approaches to treating retinal detachment
Experts in the field of ophthalmology emphasize that the successful treatment of retinal detachment depends on the type and degree of development of this condition, as well as the individual characteristics of the patient. One of the main treatment methods is surgical intervention, which may include procedures aimed at restoring the integrity of the retina, eliminating tears, and fixing the retina in the correct position. Experts also note the importance of seeking medical help early, as delays in treatment can lead to deterioration of visual function and the development of complications.
Furthermore, the development of individualized treatment plans taking into account the specifics of each particular case of retinal detachment is a key aspect of successful therapy. Experts advocate for the use of modern technologies and techniques, such as laser coagulation, pneumatic vitrectomy, and intravitreal injections, to achieve optimal results. Continuous monitoring and support from specialists help patients with retinal detachment restore visual function and prevent possible complications.

Methods for diagnosing retinal detachment
To diagnose retinal detachment, doctors typically use various methods, including ophthalmoscopy, optical coherence tomography (OCT), and retinal angiography. With ophthalmoscopy, the doctor can visually assess the condition of the retina and identify characteristic changes indicative of detachment. OCT provides detailed images of the retinal tissues and determines the extent of the retinal detachment. Retinal angiography is used to study the circulation in the eye and evaluate the condition of the vessels during the diagnosis of retinal detachment.
In addition to the aforementioned methods, other diagnostic procedures such as ultrasound of the eye or electrophysiological tests may be used, depending on the clinical situation and the need for clarification of the diagnosis. Accurate and timely diagnosis of retinal detachment is a key step in determining the optimal treatment plan and preventing potential complications, preserving the patient’s visual functions.
-
– Ophthalmoscopy: the doctor conducts a visual examination of the fundus using an ophthalmoscope to identify characteristic changes indicating retinal detachment.
– Optical coherence tomography (OCT): this method provides detailed slices of the eye structures, allowing for the assessment of the degree of retinal detachment and determining the treatment strategy.
– Retinal angiography: conducting this procedure allows studying blood flow in the eye and evaluating the condition of the vessels to determine further steps in case of retinal detachment.
– Ultrasound examination of the eye: this additional diagnostic method can be used to obtain more information about the condition of the eye structures when retinal detachment is suspected.
– Electrophysiological tests: these tests can be applied to assess the electrical activity of the retina and visual system, helping to more accurately determine the functional state of the eye in case of retinal detachment.
Effective methods for treating retinal detachment
In addition to surgical methods, the development of an individual treatment plan may include the use of medications, physiotherapy, and lifestyle modification recommendations. Careful monitoring of the patient after treatment and regular consultations with an ophthalmologist play an important role in preventing recurrences and maintaining visual function in the long term.
- Surgical intervention: Effective methods for treating retinal detachment include pneumatic retinopexy, scleral buckling, and laser photocoagulation, aimed at restoring adhesion between the retina and the vascular layer.
- Individual approach: Treating retinal detachment requires a balanced plan that considers the extent of detachment, the nature of the tears, and the overall condition of the patient’s eye.
- Medication therapy: In addition to surgical methods, the use of medications can be part of a comprehensive treatment for retinal detachment, for example, to maintain eye health after surgery.
- Physical therapy techniques: Some patients may benefit from physical procedures aimed at improving visual function and restoring the eye muscles.
- Continuous monitoring and consultations: Regular visits to an ophthalmologist after treatment play an important role in preventing complications and maintaining eye health in the future.
Measures to prevent retinal detachment
Patients with high myopic refraction or a family history of retinal detachment are advised to pay special attention to their eyes, monitor changes in visual function, and follow all of the doctor’s recommendations. A healthy lifestyle, including proper nutrition, physical exercise, and avoiding bad habits, is also important for the overall health of the eyes and visual function.
- Regular check-ups with an ophthalmologist: Visiting an ophthalmologist to check the condition of the eyes helps identify early-stage factors that predispose to retinal detachment.
- Monitoring blood pressure and vascular condition: Blood pressure levels and overall vascular health are important for preventing complications related to retinal detachment.
- Avoiding injuries and heavy physical exertion: Preventing injuries and avoiding significant physical strain help reduce the risk of retinal tears.
- Monitoring high myopic refraction: Patients with high myopic refraction are advised to carefully monitor their eye health and regularly consult a specialist.
- Healthy lifestyle: Proper nutrition, physical exercise, and avoiding bad habits contribute to overall eye health and the prevention of potential vision problems.
Fascinating aspects of retinal detachment
Thanks to modern diagnostic methods and surgical treatment, medical science continues to improve strategies for combating retinal detachment and enhancing outcomes for patients. It is also interesting how preventive measures, including regular check-ups and maintaining a healthy lifestyle, can play a key role in preventing the development of this serious eye disease.