Inguinal epidermophyte: diagnosis, treatment, and prevention
- Description of Inguinal Epidermophyte
- Etiology of Groin Epidermophyte Infection
- Clinical manifestations of Groin Epidermophytes
- Expert recommendations for the treatment of Groin Epidermophyte
- Methods of diagnosing Groin Epidermophyte Infection
- Methods of treating Groin Epidermophytosis
- Prevention Measures for Groin Epidermophyte Infection
- Amazing features of Groin Epidermophyte infection
- FAQ
Description of Inguinal Epidermophyte
Inguinal epidermophytosis, also known as a fungal infection of the groin area, is a dermatophyte infection caused by fungi of the genera Trichophyton and Epidermophyton. This infection often manifests as redness, itching, and the formation of red spots that may be moist or scaly. The main risk factors for the development of inguinal epidermophytosis include increased humidity and temperature in the groin area, wearing synthetic underwear, excessive sweating, and a history of similar infections.
To diagnose inguinal epidermophytosis, a dermatologist examination and microscopic study of the skin condition are usually conducted. Treatment typically includes the use of antifungal ointments or creams, antimycotic medications, as well as recommendations for hygiene and prevention of relapses. It is important to consult a specialist for an accurate diagnosis and to prescribe effective therapy for the successful resolution of this condition.
Etiology of Groin Epidermophyte Infection
The causes of groin epidermophytosis are often associated with a fungal infection caused by dermatophytes of the classes Trichophyton, Epidermophyton, and Microsporum. These fungi thrive in warm and humid environments, such as footwear, pools, and showers, and can affect the skin with poor hygiene. Factors that increase the risk of the disease include excessive sweating, tight clothing, a weakened immune system, as well as contact with contaminated objects or individuals, which facilitates the transmission of the infection.
- Fungal infection: Groin epidermophytosis is often associated with dermatophytes of the fungal classes Trichophyton, Epidermophyton, and Microsporum that thrive in warm and humid conditions.
- Poor hygiene: Poor hygiene creates favorable conditions for the development of fungal infections, especially with increased sweating.
- Tight clothing: Wearing tight clothing contributes to the creation of a warm and humid environment, which promotes the development and transmission of infection.
- Weakened immunity: A weakened immune system makes the body more susceptible to various infections, including fungal skin lesions.
- Contact with infected objects or people: Close contact with infected objects or people can contribute to the spread of fungal infections, including groin epidermophytosis.
Clinical manifestations of Groin Epidermophytes
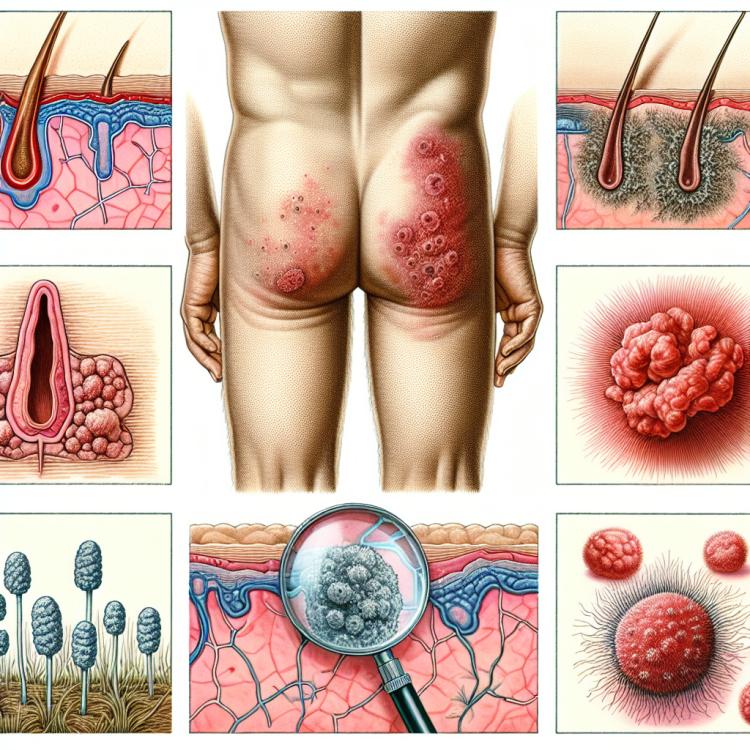
Symptoms of groin epidermophytosis include itching, redness, and peeling of the skin in the groin area. The appearance of a characteristic ring-shaped rash with clear borders, possibly with hair on the periphery, is also typical for this disease. In some cases, there may be swelling, blisters with fluid, or even ulcers. The skin can become painful and irritated, especially when in contact with aggressive substances or when rubbing against clothing.
- Itching and redness: Patients may experience intense itching and noticeable redness in the groin area.
- Peeling skin: Abundant skin peeling is observed, especially in the affected area.
- Ring-shaped rash: A characteristic symptom is the appearance of a ring-shaped rash with clear boundaries and often with hair on the periphery.
- Swelling and blisters: In some cases, skin swelling and the formation of fluid-filled blisters may occur.
- Painfulness: The skin in the groin area becomes painful and sensitive, especially when rubbed against clothing or in contact with irritating substances.
Expert recommendations for the treatment of Groin Epidermophyte
Expert recommendations for treating groin epidermophyte infections usually include the use of antifungal medications in the form of creams or ointments containing the active ingredient clotrimazole, miconazole, or terbinafine. They have the property of killing the fungi that cause the infection and contribute to the rapid recovery of the skin. Additionally, in cases of severe itching and inflammation, anti-inflammatory agents may be used to alleviate symptoms.
Experts also recommend maintaining strict hygiene in the groin area, avoiding tight synthetic clothing, which promotes better ventilation of the area and helps prevent recurrence of the infection. It is important to continue treatment even after symptoms have disappeared to prevent relapses of the disease and ensure complete recovery.

Methods of diagnosing Groin Epidermophyte Infection
Diagnosis of groin epidermophyte usually starts with a visual examination of the affected area of skin. The doctor may pay attention to characteristic symptoms such as rashes, redness, and peeling. To confirm the diagnosis, it may sometimes be necessary to take a skin sample for microscopic examination or culture for fungi. If necessary, additional laboratory diagnostics may be performed, for example, testing for fungal DNA.
- Visual inspection: The doctor examines the affected area of the skin to identify characteristic symptoms.
- Microscopic examination: Taking a skin sample to determine the presence of fungi or for subsequent culturing.
- Laboratory diagnostics: Additional blood or sample analysis to detect fungi or pathogenic DNA.
- Differential diagnosis: Exclusion of other pathologies with similar symptoms, such as allergic reactions or other fungal infections.
- Medical history: The patient’s history and facts that may influence the development of the disease are of significant importance.
Methods of treating Groin Epidermophytosis
- Use of antifungal creams and ointments: The most common treatment method for external infections, helps eliminate fungal infection.
- Systemic treatment with antifungal medications: Used in cases of severe or widespread infections, when systemic intervention is needed.
- Changing hygiene habits: Including regular washing and drying of the groin area, wearing loose clothing, and maintaining personal hygiene to prevent recurrences.
- Following the doctor’s recommendations: It is important to adhere to the doctor’s instructions on the use of medications and to monitor the treatment process for effective eradication of the infection.
- Monitoring skin condition: It is important to keep an eye on changes in skin condition, promptly consulting a doctor if symptoms worsen or complications arise.
Prevention Measures for Groin Epidermophyte Infection
- Personal hygiene compliance: daily showering, thorough drying and drying of the groin area after contact with water.
- Avoiding tight clothing: wearing loose and breathable clothing will help prevent the creation of a moist environment where a fungal infection can develop.
- Precautions when visiting public places: careful use of public pools, showers, and saunas, as well as wearing shoes in public changing rooms, can reduce the risk of infection.
- Timely treatment of other skin infections: seeing a doctor at the first signs of a skin infection will help prevent its spread and the likelihood of developing inguinal epidermophytosis.
- Avoiding contact with infected items: it is advisable to avoid contact with infected individuals or using their personal belongings to prevent the transmission of infection.
Amazing features of Groin Epidermophyte infection
Interestingly, inguinal epidermophytiasis can be transmitted through contact with infected surfaces, such as public showers and swimming pools, as well as through direct contact with already infected individuals. This highlights the importance of following preventive measures and maintaining proper hygiene to prevent the disease.