Paraproctitis: diagnosis, treatment, and prevention
- Definition and causes of paraproctitis
- Etiology of paraproctitis
- The clinical picture of paraproctitis
- Expert opinion on methods of treating paraproctitis
- Methods for diagnosing paraproctitis
- Approaches to the treatment of paraproctitis
- Preventive measures for paraprocititis
- Amazing facts about paraproctitis
- FAQ
Definition and causes of paraproctitis
Paraproctitis is an inflammatory process in the perianal area that can be caused by an infection in the anal glands or trauma. The main cause of paraproctitis is infection caused by various pathogenic microorganisms, such as staphylococci, streptococci, and intestinal bacteria.
Paraproctitis often develops due to incomplete free drainage of secretion from the rectum, which promotes the growth of microorganisms in the surrounding tissues. In addition, trauma, a sedentary lifestyle, dietary factors, and a weakened immune system can also contribute to the development of paraproctitis.
Etiology of paraproctitis
Paraproctitis, characterized by inflammation of the perirectal tissue, is usually caused by a bacterial infection. The main pathogens causing paraproctitis are anaerobic and aerobic bacteria, including Escherichia coli, Streptococcus, and Staphylococcus aureus. The occurrence of paraproctitis is often associated with violations of hygiene standards, injuries around the anorectal area, or underlying diseases that contribute to the development of infection.
- Bacterial infection: Paraproctitis is often caused by bacterial inflammation of the perirectal tissue, usually by anaerobic and aerobic bacteria.
- Poor hygiene: Insufficient hygiene around the anus can contribute to the development of an infection leading to paraproctitis.
- Injuries: Mechanical damage in the anorectal area can be a cause of paraproctitis.
- Comorbid conditions: Certain conditions, such as diabetes or immunodeficiency states, increase the risk of developing paraproctitis.
- Obstruction of anal glands: Obstruction by secretions in the anal glands can lead to the development of an infection and, ultimately, to paraproctitis.
The clinical picture of paraproctitis
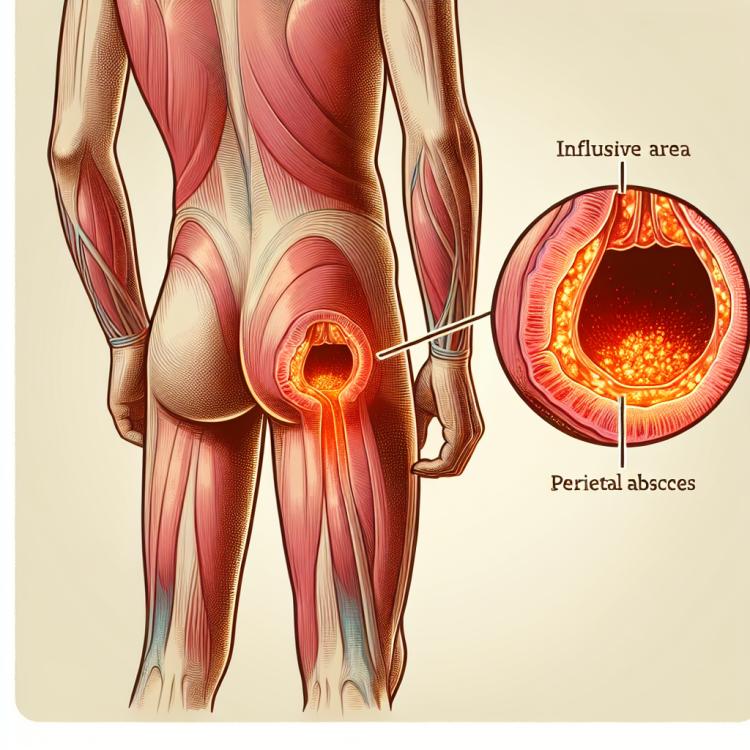
Patients with paraproctitis often present with characteristic symptoms such as pain and swelling in the area of the rectum, as well as an elevated body temperature. Patients may also exhibit redness and infiltration of the tissues around the anus, which is associated with an inflammatory reaction. In some cases, paraproctitis can lead to the formation of an abscess in this area, accompanied by an intensification of pain and a deterioration of the patient’s overall condition.
- Pain and swelling: are characterized by tenderness and an increase in the volume of tissue in the area of the rectum.
- Increased body temperature: is often observed in patients with paraproctitis and is associated with the inflammatory process.
- Redness and infiltration of tissues: are caused by the inflammatory reaction around the anus.
- Abscess formation: in some cases, paraproctitis may lead to the formation of an abscess, accompanied by increased pain and a general deterioration of condition.
- Bowel disturbances: patients with paraproctitis may experience difficulties with defecation due to pain and discomfort in the anus.
Expert opinion on methods of treating paraproctitis
Various treatment methods for paraproctitis may be recommended depending on the severity of the condition and the presence of complications. Experts emphasize the importance of timely consultation with a doctor for accurate diagnosis and the establishment of an optimal treatment plan. In some cases, surgical intervention may be required to drain the abscess or remove the affected tissue, followed by the use of antibiotics. However, conservative treatment, including the use of antibiotics, may be effective in milder cases of paraproctitis without abscess formation.

Methods for diagnosing paraproctitis
For the diagnosis of paraproctitis, it is important to conduct a visual examination of the anus and surrounding tissues, as well as an assessment for signs of inflammation and swelling. Additional methods, such as ultrasound or magnetic resonance imaging, may be used to determine the extent of the process and identify potential complications, such as abscess.
Laboratory methods, including a complete blood count and biochemical tests, can help establish the presence of inflammation and infection markers. Additionally, bacteriological analyses of swabs from the affected area may be conducted to identify the causative agents of the infection and determine their sensitivity to antibiotics.
- Visual examination: The doctor examines the area around the anus and the surrounding tissues for signs of inflammation and swelling.
- Ultrasound examination: This method can be used to determine the extent of the infectious process and identify possible complications, such as abscesses.
- Magnetic resonance imaging (MRI): MRI helps to obtain a more detailed image of the rectal area and surrounding tissues.
- Complete blood count: A laboratory test that can show signs of inflammation and the presence of infection in the body.
- Bacteriological analysis of smears: This method can identify the causative agents of infection and determine their sensitivity to antibiotics.
Approaches to the treatment of paraproctitis
In addition, adherence to hygiene measures is recommended, along with the use of local anti-inflammatory medications, as well as pain and swelling relief. In chronic paraproctitis, it is important to identify the underlying cause of the disease and conduct appropriate treatment to prevent recurrences.
- Abscess drainage: In the case of acute paraproctitis with abscess formation, surgical drainage may be required to remove purulent material and reduce pressure in the inflamed tissues.
- Antibiotic therapy: The use of antibiotics may be necessary to combat the infection and prevent its spread, especially in cases of complicated paraproctitis.
- Anti-inflammatory medications: The use of topical anti-inflammatory agents can help reduce inflammation and pain in the affected area.
- Adherence to hygiene measures: Regular washing of the affected area, using soft paper products, and hygiene pads contribute to the improvement of the condition and prevention of paraproctitis recurrences.
- Local anesthesia: Various local anesthetics and anti-inflammatory medications in the form of ointments or creams may be used to alleviate pain and swelling.
Preventive measures for paraprocititis
Additionally, maintaining a healthy lifestyle, proper nutrition, strengthening the immune system, and timely treatment of other diseases that lead to intestinal disorders can also help reduce the risk of paraproctitis. Regular medical check-ups and consultations with specialists can also help identify problems at an early stage and take the necessary measures for their prevention.
- Regular adherence to anal hygiene, including washing after defecation, helps prevent bacterial infections.
- Avoiding injuries and mechanical damage in the anorectal area contributes to preventing inflammatory processes.
- Maintaining a healthy lifestyle, a balanced diet, and strengthening the immune system help bolster the body’s defenses.
- Avoiding hypothermia of the anorectal area helps prevent the development of inflammatory diseases.
- Regular preventive check-ups with specialists allow for the identification of potential problems at early stages and taking measures to prevent them.
Amazing facts about paraproctitis
One interesting fact about paraproctitis is that the leading role in the development of this disease is played by the microflora of the surrounding tissues, which penetrates the per rectal space through affected fat cells or rectal channels. It is also important to remember that paraproctitis can occur both independently and as a complication of other diseases or conditions, such as blood stagnation in the pelvic area or the presence of tumors.