Pathological fracture: mechanisms of occurrence and approaches to treatment
- Understanding the nature of a pathological fracture
- Etiology of pathological fracture
- Clinical picture of pathological fracture
- Forecast and recommendations for the treatment of pathological fracture
- Methods for diagnosing pathological fractures
- Methods of treating pathological fracture
- Prevention of pathological fractures
- Amazing aspects of pathological fractures
- FAQ
Understanding the nature of a pathological fracture
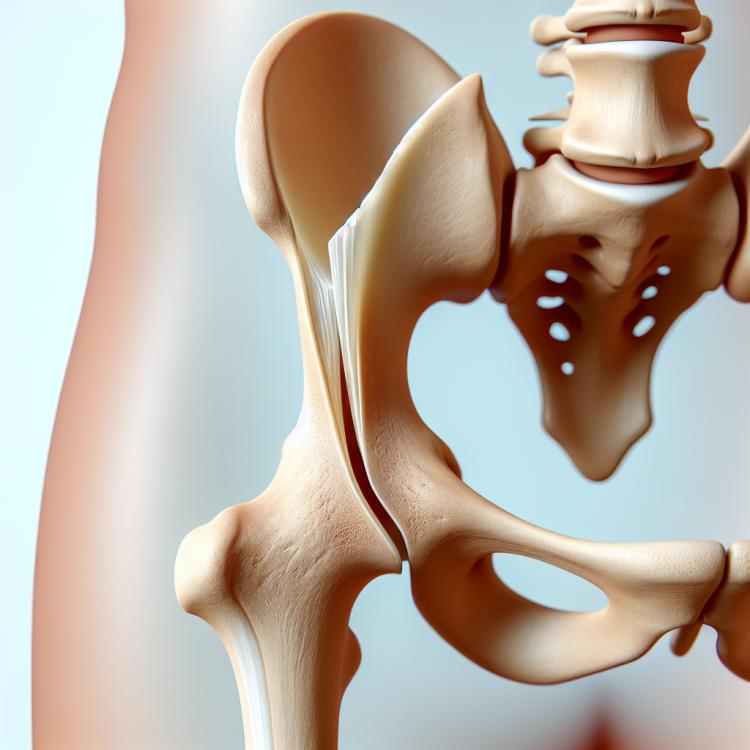
A pathological fracture is a special category of fracture caused by weakening and changes in the bone structure due to a pathological process or disease. This type of fracture can occur as a result of osteoporosis, bone tumors, infectious lesions, or developmental anomalies. A pathological fracture differs from a traumatic one in that it arises from changes in bone tissue rather than mechanical impact on the bone.
Studying the nature of pathological fractures is crucial for developing optimal methods for the diagnosis and treatment of this condition. Understanding the factors that contribute to the development of pathological fractures allows for a comprehensive approach to their treatment, including pharmacotherapy, surgical intervention, or other methods, depending on the underlying disease and the nature of the bone injury.
Etiology of pathological fracture
The main causes of pathological fractures include osteoporosis, bone cancer, metastases, and bone infections. Osteoporosis, a chronic disease characterized by a decrease in bone mass and structural support of the bone, puts patients at high risk for fractures. Patients with bone cancer or metastases have an increased risk of developing pathological fractures due to disruptions in the structure and strength of bones caused by the tumor process. Therefore, it is important to consider these factors in the diagnosis and treatment of pathological fractures.
- Osteoporosis: Decreased bone mass and structural changes increase the risk of fractures.
- Bone cancer: Cancerous processes can destroy bone and contribute to its brittleness.
- Metastases: The spread of cancer cells to the bones can cause their destruction and result in pathological fractures.
- Bone infections: Inflammatory processes in the bone can complicate its structure and lead to fractures.
- Acute and chronic trauma exposure: Bone damage can weaken it and lead to pathological fractures.
Clinical picture of pathological fracture
The clinical picture of a pathological fracture may include pain in the area of the fracture, swelling, changes in the shape or position of the joint, as well as limited movement in the damaged area. Patients may experience increased pain with load or movement, as well as changes in the range of motion in the fracture zone. In some types of fractures, such as compression fractures of the spine, there is an added risk of spinal cord injury, which may manifest as weakness or loss of sensation, disturbances in the functions of pelvic organs, and sensitivity of the lower extremities.
- Pain in the area of the fracture: patients may experience sharp or dull pain at the fracture site, often increasing with movement.
- Swelling and edema: the appearance of swelling and increase in the volume of tissues around the fracture, which may be noticeable visually and palpable.
- Change in the shape or position of the joint: a fracture may be accompanied by deformity of the limb or alteration of the joint’s position.
- Limitation of movement: resulting limitation of movement in the area of the fracture due to pain sensations or structural damage to the tissues.
- Increased pain with load: pain syndrome may intensify with attempts to move or when pressure is applied to the damaged area.
Forecast and recommendations for the treatment of pathological fracture
Experts claim that the prognosis of a pathological fracture depends on its location, severity, and the overall condition of the patient. The primary goal is to restore function to the bone and to prevent the recurrence of the fracture. Various methods are used in the treatment of pathological fractures, including conservative approaches with the use of drug therapy and rehabilitation procedures, as well as surgical interventions when necessary. A personalized approach that takes into account the specifics of each case allows for the best outcomes in the treatment of pathological fractures.

Methods for diagnosing pathological fractures
For the diagnosis of pathological fractures, X-ray, computed tomography (CT), and magnetic resonance imaging (MRI) are often used. X-ray is the primary diagnostic method, allowing visualization of changes in the bones and detection of fractures. CT and MRI provide a more detailed image of tissues and allow for a more accurate assessment of pathological changes, especially in cases where it is necessary to evaluate the condition of surrounding tissues.
-
– X-ray: a method for diagnosing pathological fractures, allowing visualization of changes in the bones.
– Computed Tomography (CT): a more detailed diagnostic method that provides comprehensive information about the condition of bones and tissues.
– Magnetic Resonance Imaging (MRI): a high-resolution method that allows for a more detailed assessment of the condition of bones and surrounding tissues.
– Bone Scintigraphy: a method using radioactive substances to detect areas with altered metabolism, such as tumors or inflammation.
– Biopsy: an invasive diagnostic method that can be used to obtain a tissue sample for a more accurate determination of the pathological process.
Methods of treating pathological fracture
- Conservative treatment: Includes the fixation of the fracture using a cast or orthosis, which helps bone healing in the correct position.
- Rehabilitation activities: An important part of treatment, including physical therapy and exercises to restore strength and mobility of the affected area.
- Hospital observation: Patients may require prolonged inpatient monitoring to control the healing process and to prevent complications.
- Surgical intervention: Necessary in cases where the fracture cannot be addressed with conservative methods, such as with displaced or non-mobile fractures.
- Use of medications: Includes analgesics, antibiotics in the presence of infection, and medications to improve bone regeneration.
Prevention of pathological fractures
- Nutrition and Vitamins: Regular consumption of foods rich in calcium and vitamin D contributes to strengthening bones and may reduce the risk of pathological fractures.
- Moderate Physical Activity: Regular exercises such as walking, swimming, or yoga help strengthen muscles and bones, which helps prevent fractures.
- Avoiding Harmful Habits: Quitting smoking and moderate alcohol consumption reduce the risk of osteoporosis and pathological fractures.
- Regular Medical Check-ups: Timely consultation with a doctor and checking bone density can help identify early signs of osteoporosis and prevent possible fractures.
- Adhering to Medication Regimen: Patients at risk for pathological fractures should strictly follow doctors’ recommendations for taking medications to prevent osteoporosis and other conditions that increase the risk of fractures.