Understanding Pericarditis: Causes, Symptoms, and Treatment Methods
Understanding pericarditis: symptoms, causes, and treatment
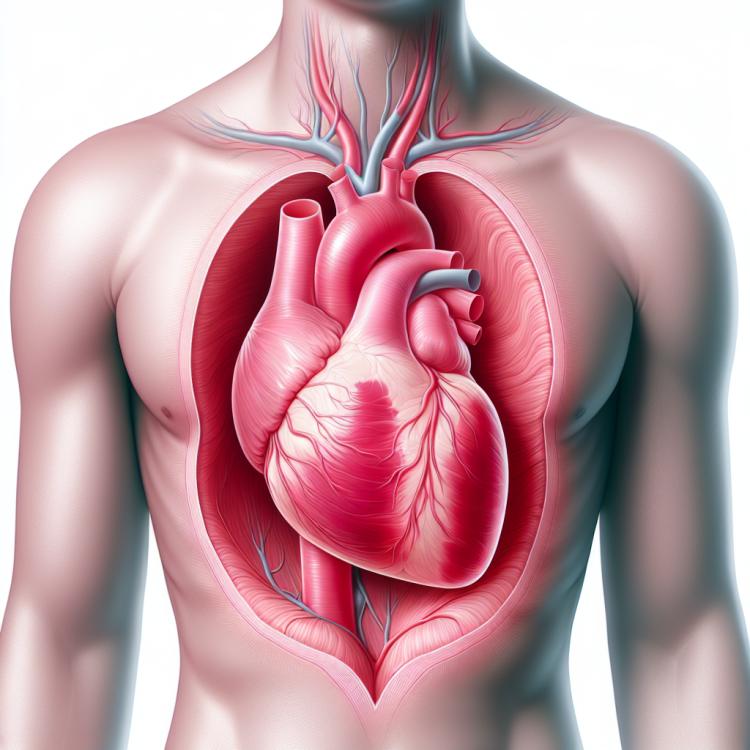
Pericarditis is an inflammatory disease of the heart’s membrane, most often caused by viral infections or autoimmune reactions. The main symptoms of pericarditis are chest pain, worsening with deep breathing or swallowing, as well as shortness of breath. Diagnosis includes physical examination, electrocardiogram, and echocardiography.
Treatment of pericarditis depends on its cause; however, it usually involves the use of anti-inflammatory drugs such as NSAIDs and treatment of the underlying condition if one exists. In cases where pericarditis becomes chronic or leads to complications, surgical intervention in the form of pericardiectomy may be required.
Etiology of pericarditis
Pericarditis is an inflammatory disease of the heart’s outer layer, known as the pericardium. Its causes can be diverse, including infections, autoimmune processes, cancer, and drug complications. Infectious agents such as viruses (e.g., Epstein-Barr virus, herpes simplex virus) or bacteria (e.g., staphylococcus or streptococcus) are among the main causes of pericarditis. Autoimmune causes, including rheumatoid arthritis or systemic lupus erythematosus, can also contribute to the development of this disease.
Other causes of pericarditis may include trauma, lung cancer, metastases of tumors to the pericardium, drug complications (e.g., chemotherapy drugs), and idiopathic factors. Establishing the exact cause of pericarditis is crucial for choosing the optimal treatment method and predicting the outcomes.
- Infections: viruses (for example, Epstein-Barr virus, herpes simplex virus) and bacteria (for example, staphylococcus or streptococcus) are often causes of pericarditis.
- Autoimmune diseases: rheumatoid arthritis, systemic lupus erythematosus, and other autoimmune processes can contribute to inflammation of the pericardium.
- Trauma: injuries to the heart and pericardium resulting from trauma or surgical intervention can cause pericarditis.
- Oncological diseases: lung cancer, metastases of tumors in the pericardium, and chemotherapy may be associated with the development of pericarditis.
- Drug complications: some medications, including certain chemotherapy drugs and anti-inflammatory agents, can cause pericarditis as a side effect.
Clinical manifestations of pericarditis
Clinical manifestations of pericarditis may include chest pain that can worsen with deep breathing or swallowing. Patients often describe this pain as sharp or burning, allowing the doctor to differentiate it from pain caused by other reasons. Additionally, pericarditis may present with shortness of breath, fatigue, decreased physical activity, increased heart rate, and possible signs of arrhythmia.
Symptoms related to an elevated body temperature, deterioration of general condition, fatigue, and anorexia may also occur. It is important to note that the clinical picture of pericarditis can be diverse and depend on the degree of inflammation, the underlying cause of the disease, and the presence of complications. A comprehensive examination is necessary to establish a diagnosis, including physical and laboratory examinations, ECG, echocardiography, and other diagnostic methods.
- Chest pain: sharp or burning pain that may worsen with deep breathing or swallowing.
- Shortness of breath: difficulty breathing that may worsen with physical exertion or when lying down.
- Fatigue: a sense of extreme tiredness even with minimal exertion, which may be related to a decrease in overall body tone.
- Increased heart rate: an accelerated heart rhythm, which may be due to increased activity of the sympathetic nervous system in response to the inflammatory process.
- Heartbeat irregularities: possible arrhythmias or irregular heart rhythms, such as tachycardia or extrasystoles, may be symptoms of pericarditis.
Expert opinions on the treatment of pericarditis
The treatment of pericarditis requires a comprehensive approach based on the etiology and clinical course of the disease. Expert opinions on the treatment of pericarditis emphasize the importance of identifying the causal factor to prescribe optimal therapy. Medication treatment typically includes the use of anti-inflammatory drugs, such as NSAIDs and steroids, as well as antibiotics in the case of infectious etiology of the disease.
Experts also note the importance of monitoring patients after treatment to assess the effectiveness of the measures taken and to prevent possible complications. If necessary, surgical intervention may be required, such as pericardial drainage or pericardectomy, which also demands an individualized approach and specialized medical intervention.

Diagnosis of pericarditis
The diagnosis of pericarditis includes a wide range of methods and studies, starting from physical examination and gathering medical history to more complex medical procedures. The doctor assesses the symptoms and complaints of the patient, examines the heart sounds using a stethoscope, and conducts an examination to identify possible signs of inflammation of the pericardium.
Additional diagnostic methods include an ECG, which can show characteristic changes in heart rhythm and conductivity, as well as echocardiography, which allows visualization of heart structures and assessment of the presence of inflammatory changes in the pericardium. Laboratory tests, such as blood tests for inflammatory markers, may also be conducted to confirm the diagnosis and evaluate the degree of inflammation.
- Physical examination: The doctor conducts an examination, assessing symptoms, heart sounds, and possible signs of pericardial inflammation.
- Electrocardiography (ECG): A method for recording the electrical activity of the heart, allowing the detection of changes in heart rhythm and conductivity.
- echocardiography (ultrasound of the heart): A visualization method that allows the assessment of heart structures, the pericardium, and the detection of inflammatory changes.
- Laboratory blood tests: Conducted to assess the level of inflammatory markers, such as C-reactive protein and others.
- Magnetic resonance imaging (MRI) and computed tomography (CT): Additional visualization methods that can be used for further diagnosis of disease characteristics.
Treatment of pericarditis
In some cases, especially with chronic or recurrent pericarditis, a decision may be made to perform surgical intervention, such as pericardiocentesis or pericardiectomy. It is important to approach the treatment of pericarditis individually, taking into account the characteristics of each clinical case and conducting comprehensive monitoring of the patient.
- Anti-inflammatory medications: prescribed to reduce inflammation in the pericardium and alleviate symptoms.
- Antibiotics or antiviral medications: used in pericarditis caused by infection to eliminate the pathogen.
- Drainage of fluid: in cases of excess fluid in the pericardium, drainage may be necessary to ease breathing and cardiac function.
- Surgical intervention: in some cases of chronic or recurrent pericarditis, surgery may be required, such as pericardiocentesis or pericardiectomy.
- Personalized approach: it is important to consider the treatment of pericarditis taking into account the individual characteristics of each patient and to provide comprehensive monitoring of their condition.
Prevention of pericarditis
Preventing autoimmune diseases, timely and proper treatment of infections, controlling risk factors for cardiovascular diseases, and leading a healthy lifestyle, including a balanced diet and physical activity, can help reduce the likelihood of developing pericarditis. It is also important to pay attention to the symptoms of the disease and seek medical help at the first signs of heart problems.
- Maintaining a healthy lifestyle: Leading an active lifestyle, consuming nutritious foods, refraining from harmful habits, and having regular medical check-ups help maintain cardiovascular health.
- Infection prevention: Avoiding contact with people suffering from infectious diseases, proper handwashing, and adherence to other hygiene rules reduce the risk of infection from various pathogens, preventing the possible development of pericarditis.
- Vaccination: Following the vaccination schedule and getting immunized against infectious diseases helps strengthen the immune system and prevent the risk of pericarditis caused by specific pathogens.
- Limiting autoimmune reactions: Monitoring autoimmune diseases, taking medications aimed at stabilizing the immune system, and timely consulting a doctor upon the appearance of characteristic symptoms help prevent the development of pericarditis.
- Seeking medical help: If characteristic symptoms arise, it is necessary to consult a doctor for timely diagnosis and treatment of pericarditis, which will help prevent complications and disease progression.
Amazing aspects of pericarditis
Another interesting aspect of pericarditis is its clinical presentation, which can range from mild or absent symptoms to a serious condition requiring immediate intervention. Understanding the various manifestations of pericarditis and their timely diagnosis is essential for effective management of this disease and preventing possible complications.