Barrett’s Esophagus: Diagnosis, Complications, and Prevention
- Main aspects of Barrett’s esophagus
- Risk factors for the development of Barrett’s Esophagus
- Signs and manifestations of Barrett’s esophagus
- The specialists’ perspective on the treatment methods for Barrett’s Esophagus
- Modern methods of detecting Barrett’s esophagus
- Recommendations for the treatment of Barrett’s Esophagus
- Measures for the prevention of Barrett’s Esophagus
- Amazing Aspects of Barrett’s Esophagus
- FAQ
Main aspects of Barrett’s esophagus
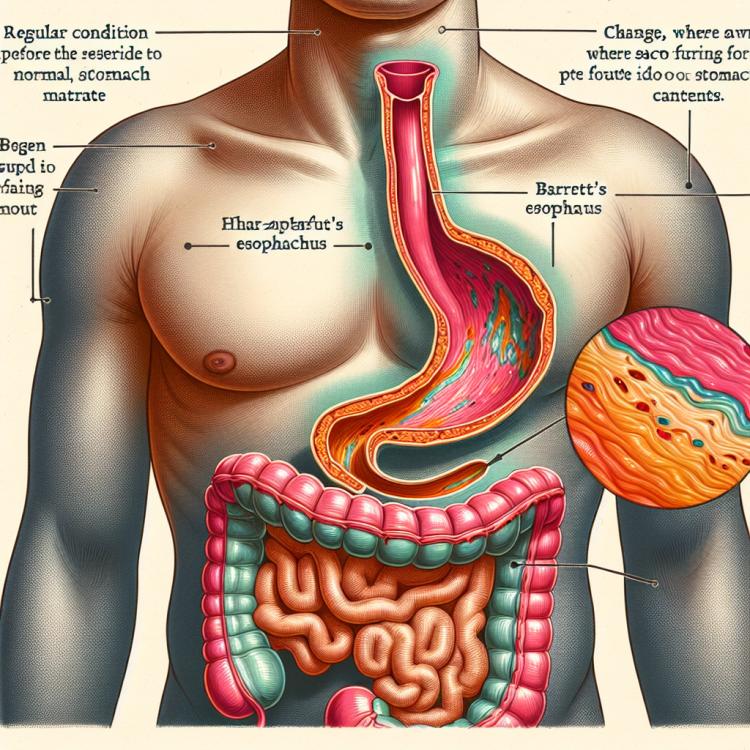
Barrett’s esophagus is a condition characterized by the replacement of the normal flat epithelial tissue of the esophagus with cuboidal epithelial tissue. This change typically occurs in response to chronic exposure to stomach acid due to gastroesophageal reflux. Barrett’s esophagus is a precancerous condition that increases the risk of developing esophageal adenocarcinoma, so early detection and management of this condition play a crucial role in the prevention of esophageal cancer.
Risk factors for the development of Barrett’s Esophagus
The development of Barrett’s Esophagus is associated with various risk factors, including chronic heartburn, which is the most common symptom of this condition. Gastroesophageal reflux disease, where the stomach contents are regularly pushed back into the esophagus, can lead to changes in the esophageal epithelium, promoting the development of Barrett’s Esophagus.
Other factors, including obesity, smoking, age over 50, a hereditary predisposition, and long-term use of certain medications, can also increase the likelihood of developing Barrett’s Esophagus. It is important to be aware of these risks and take appropriate measures for prevention and timely intervention if necessary.
- Chronic heartburn: The periodic return of stomach contents to the esophagus can irritate it and lead to the development of Barrett’s Esophagus.
- Gastroesophageal reflux disease: Regular backflow of stomach contents into the esophagus contributes to changes in the tissues of the esophagus.
- Obesity: Excess weight can increase pressure in the abdominal cavity, promoting acid reflux from the stomach into the esophagus.
- Smoking: Nicotine and other harmful substances in cigarette smoke can weaken the sphincter between the esophagus and stomach, intensifying reflux.
- Age over 50: The risk of developing Barrett’s Esophagus increases with age due to the natural aging of the body and its ability to regenerate tissues.
Signs and manifestations of Barrett’s esophagus
Symptoms of Barrett’s esophagus can vary and are associated with changes in the esophageal epithelium. Patients may experience chronic heartburn, a feeling of tightness in the chest, frequent belching, and discomfort when swallowing. Some people may also complain of chest or abdominal pain, as well as nonspecific complaints related to dysphagia or difficulty swallowing food. Given the potentially dangerous consequences of Barrett’s esophagus, it is important to see a doctor at the first signs of esophageal dysfunction and to undergo gastroscopy for diagnosis.
- Chronic heartburn: a constant burning sensation in the chest area, often occurring after eating.
- Discomfort when swallowing: discomfort or pain when swallowing food, feeling of food getting stuck in the esophagus.
- Belching: regular return of food or liquid from the stomach to the oral cavity during or after eating.
- Chest or abdominal pain: unpleasant sensations in the chest or abdominal area, not typical of other conditions.
- Dysphagia: difficulty or pain when swallowing, possibly with the sensation of food or liquid getting stuck in the esophagus.
The specialists’ perspective on the treatment methods for Barrett’s Esophagus
Experts agree that the treatment of Barrett’s esophagus should be individualized and focused on eliminating gastroesophageal reflux. One of the primary methods of therapy is the use of proton pump inhibitors to reduce gastric acid production, which aids in the healing of the esophageal epithelium and decreases the risk of progression to more serious complications.
Experts also emphasize the importance of regular monitoring of patients with Barrett’s esophagus, including performing endoscopic examinations to check the esophageal epithelium and identify precancerous changes. The potential application of surgical techniques is discussed in cases where conservative treatment is ineffective or does not yield the desired results. Timely and comprehensive intervention in the treatment of Barrett’s esophagus can significantly improve the disease prognosis and reduce the risk of developing its complications.

Modern methods of detecting Barrett’s esophagus
Modern diagnosis of Barrett’s esophagus includes performing gastroscopy with biopsy, allowing doctors to assess the condition of the esophageal epithelium at the micro level and identify the presence of dysplasia or carcinoma. Special educational diagnostic methods, such as chromoscopy or remote endoscopic imaging, may also be used to complement the information obtained from classical gastroscopy. Thorough diagnosis is a key step in managing Barrett’s esophagus, as it enables timely determination of the degree of changes and the development of an individualized treatment plan for the patient.
- Gastrointestinal endoscopy with biopsy: a key diagnostic method that allows for visual assessment of the esophagus and the collection of tissue samples for biopsy.
- Chromoscopy: a special diagnostic method that allows for a more detailed examination of the structure and nature of changes in the esophageal epithelium.
- Remote endoscopic imaging (DEI): an innovative technology that enables the capture of high-quality images of the esophagus for a more accurate assessment of tissue conditions.
- PCR tests for genetic mutations: the use of molecular genetic methods allows for the detection of certain genetic changes that may be associated with the development of Barrett’s Esophagus.
- Double contrast radiographic examination: this method allows for the visualization of changes in the esophagus using contrast agents and X-ray radiation for more detailed diagnostics.
Recommendations for the treatment of Barrett’s Esophagus
- Individualized approach: Treatment of Barrett’s esophagus should be tailored to the specifics of each individual case, including the degree of dysplasia, the presence of complications, and comorbid conditions.
- Endoscopic procedures: For patients with significant dysplasia or structural anomalies in the esophagus, endoscopic interventions such as ablation or endoscopic mucosal resection may be required.
- Surgical treatment: In some cases with a high risk of disease progression, surgical removal of part or all of the affected area of the esophagus may be recommended.
- Medication therapy: The use of medications such as anti-reflux drugs or drugs to suppress gastric acid secretion may be part of a comprehensive treatment plan.
- Regular monitoring and control: Patients with Barrett’s esophagus may be scheduled for regular endoscopic examinations to monitor treatment effectiveness and timely detection of potential complications.
Measures for the prevention of Barrett’s Esophagus
- Adhering to a healthy lifestyle, including quitting smoking and moderate alcohol consumption.
- Maintaining a healthy weight and regular physical exercise to prevent obesity, which can increase the risk of Barrett’s Esophagus.
- Avoiding spicy, acidic, or fatty foods, as well as other potentially irritating products, which can help reduce reflux and esophageal dysfunction.
- Managing chronic heartburn and other reflux symptoms by systematically taking recommended medications and consulting a doctor if conditions worsen.
- Regular check-ups and endoscopic examinations for the timely detection of changes in the esophageal epithelium and the prevention of Barrett’s Esophagus.