Pleuris: causes, symptoms, and treatment methods
Understanding pleurisy: key aspects
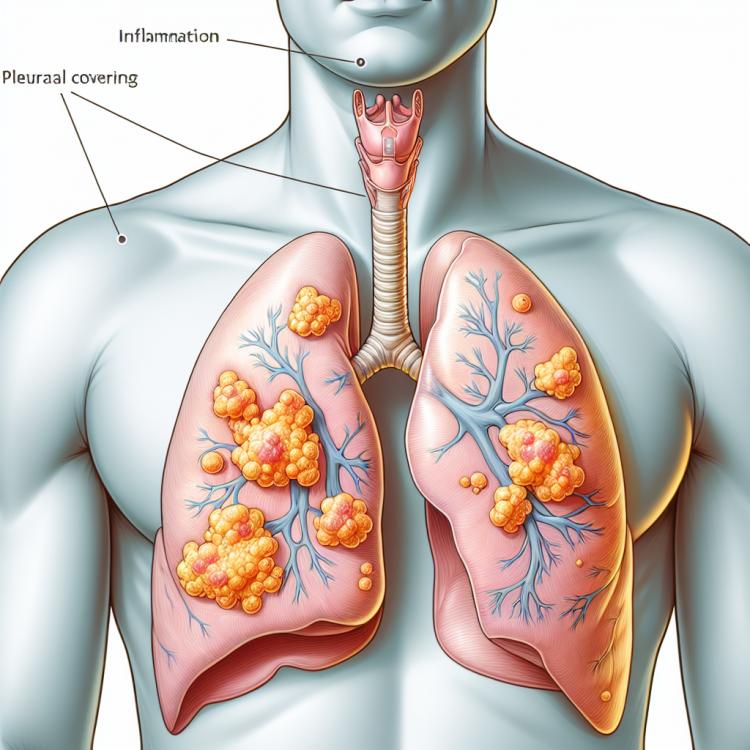
Pleurisy is an inflammatory disease of the pleura, the membrane surrounding the lungs. The main symptoms include chest pain that worsens with breathing, shortness of breath, and cough. Diagnosis is made based on clinical signs, as well as through chest X-rays or CT scans. Treatment of pleurisy depends on its cause, but typically includes the use of anti-inflammatory medications and antibiotics, and in some cases, drainage of the pleural cavity may be required.
Etiology of pleurisy
Pleura, inflammation of the lung membranes, can have various causes. The main etiological factors are infections, including bacterial, viral, or fungal, as well as autoimmune diseases such as rheumatoid arthritis. Other causes include trauma to the chest area, tumor processes, and a number of medications that can trigger the development of pleuritis. A clear definition of the causes of pleuritis plays a key role in selecting the optimal treatment and predicting outcomes.
- Infections: Pleural effusion can be caused by bacterial, viral, or fungal infections, such as pneumococcal infection.
- Autoimmune diseases: Rheumatoid arthritis or systemic lupus erythematosus can trigger the development of pleuritis.
- Chest trauma: Injuries or bruises in the chest area can lead to inflammation of the pleura.
- Neoplastic processes: Malignant tumors in the chest cavity can be associated with the development of pleuritis.
- Medications: Some medications, such as chemotherapy drugs or certain antibiotics, may be a risk factor for pleuritis.
The clinical picture of pleurisy
The clinical picture of pleurisy usually includes characteristic symptoms such as chest pain that worsens with deep breathing or coughing, as well as shortness of breath or a feeling of heaviness in the chest. Patients may sometimes experience a dry and irritating cough, as well as general weakness and fatigue.
The diagnosis of pleurisy is based on the examination of the patient, history, clinical symptoms, and instrumental investigation methods, such as chest X-ray, computed tomography, and laboratory tests. Early detection and proper treatment of pleurisy significantly impact the prognosis of the disease and prevent the development of complications.
- Chest pain: often worsening with deep breathing or coughing, can be one of the early signs of pleurisy.
- Shortness of breath: the feeling of rapid breathing or heaviness in the chest may accompany pleurisy and worsen during physical activity.
- Cough: usually dry and irritating, may occur as a reaction to the inflammation of the lung membranes in pleurisy.
- General weakness: patients often feel fatigued and unwell, which may be related to intoxication or stress on the body due to pleurisy.
- Fever: a rise in body temperature is possible in cases of infectious pleurisy, which is a typical sign of an inflammatory process.
Approaches to the treatment of pleurisy: expert opinions
Experts agree that effective treatment of pleurisy includes the use of antibiotics in the case of a bacterial infection, anti-inflammatory medications to reduce inflammation, and analgesics to relieve pain. Additionally, procedures for draining the pleural cavity and physiotherapy may be used to improve respiratory function.
It is important to individualize treatment depending on the etiology and clinical manifestations of pleurisy. Experts also emphasize the importance of regular monitoring of the patient’s condition, tracking the dynamics of the disease, and timely adjustment of therapy. A comprehensive approach to the treatment of pleurisy, based on collective experience and scientific data, contributes to increased therapy effectiveness and improved disease prognosis.

Methods of diagnosing pleurisy
The diagnosis of pleuritis involves the use of various clinical and instrumental methods to confirm the diagnosis and determine the cause of the disease. Usually, the doctor starts with a thorough medical history and physical examination, paying attention to characteristic symptoms such as chest pain, shortness of breath, and cough. To confirm the diagnosis of pleuritis, the doctor may order a chest X-ray, computed tomography (CT), or magnetic resonance imaging (MRI) to obtain a more detailed view of the condition of the lungs and pleura.
Additional diagnostic methods may include laboratory tests, such as blood and sputum analysis, to determine the possible presence of infection or inflammation. When pleuritis is suspected, it is important to conduct a comprehensive diagnosis to determine the optimal treatment strategy and prevent possible complications.
- Physical examination: the doctor examines the patient with an emphasis on pain points in the chest and assesses the overall health condition.
- Chest X-ray: helps identify inflammatory changes in the lungs and pleura, assesses the volume of fluid in the pleural cavity.
- Computed tomography (CT): used to obtain more detailed images of the lungs and pleura, allows for the detection of tumors or abscesses.
- Magnetic resonance imaging (MRI): may be performed for additional visualization of the structures of the chest and assessment of the condition of the pleura.
- Laboratory tests: include blood and sputum tests to determine the presence of infection or inflammation, as well as to assess the overall condition of the patient.
Methods of treating pleurisy
In addition, for pleuritis caused by autoimmune diseases, immunosuppressive drugs may be used. Surgical intervention may be necessary if pleuritis is due to a tumor or other anomalies in the thoracic cavity. A comprehensive approach to the treatment of pleuritis includes not only treating the underlying disease but also symptomatic therapy to alleviate symptoms and improve the patient’s quality of life.
- Antibiotic therapy: is used for infectious pleuritis with the aim of eliminating the infectious agent.
- Anti-inflammatory medications: help reduce inflammation and alleviate the symptoms of pleuritis.
- Analgesics: are used to relieve the pain syndrome associated with pleuritis.
- Immunosuppressive therapy: may be necessary in pleuritis caused by autoimmune diseases.
- Surgical intervention: may be required in the presence of a tumor or other anomalies in the thoracic cavity causing pleuritis.
Prevention of pleurisy
For individuals at risk of developing pleuritis, such as patients with chronic respiratory diseases or immunodeficiency, consultation with a doctor is recommended to develop an individual prevention strategy. Regular medical check-ups and maintaining overall health also contribute to the prevention of pleuritis and its occurrence.
- Proper respiratory hygiene: regular ventilation of premises, wet cleaning, and avoiding overheating and overcooling contribute to maintaining the health of the respiratory system.
- Vaccination: timely vaccination services, including vaccination against infection pathogens, help strengthen immunity and prevent pneumonia, one of the frequent causes of pleurisy.
- Avoiding smoking: active and passive smoking negatively impacts the condition of the lungs, increasing the risk of developing respiratory infections and pleurisy.
- Physical activity: regular moderate physical exercise helps strengthen immunity and the overall health of the body, which helps prevent the development of various respiratory diseases.
- Enhancing the body’s defenses: a balanced diet, intake of vitamins, minerals, and strengthening supplements, as well as adherence to a work and rest regimen, contribute to the overall strengthening of the body and its defenses against infections.
Interesting aspects of pleurisy
An interesting aspect of pleurisy is its diversity of causes and factors contributing to its development. This disease can be both acute and chronic, which affects the choice of treatment methods and the prognosis of the disease. Studying the many aspects of pleurisy helps expand the understanding of this disease and the development of new methods for diagnosis and treatment.