Flat feet: diagnosis, causes, and modern treatment methods
Basics of flatfoot: understanding the problem
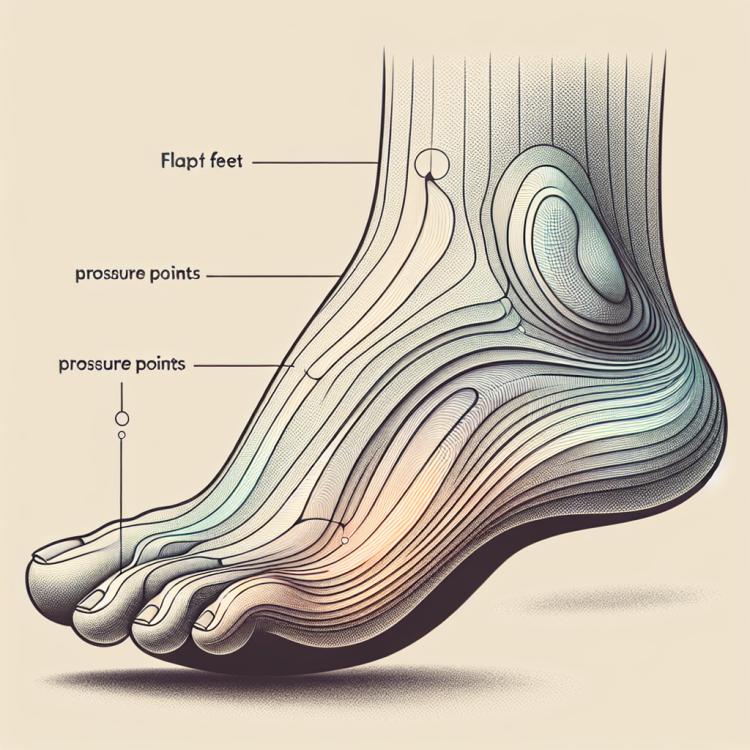
Flatfoot is a structural and/or functional change in the foot, characterized by a reduction of the arch. This condition can be congenital or acquired as a result of injuries, poor-quality footwear, or other factors that influence the structure of the foot. A person with flatfoot often experiences discomfort while walking due to improper weight distribution on the foot, which in turn can lead to pain in the legs, knees, and back.
Understanding the essence of flatfoot is significantly important for determining appropriate treatment. Doctors usually conduct a detailed examination of the foot, including assessment of anatomical features, study of symptoms, and possible causes of this condition. Determining the type and degree of flatfoot allows for the prescription of effective treatment, which may include wearing special footwear, orthopedic insoles, physical therapy, or in some cases, surgical intervention.
Etiology of flatfoot
Flatfoot is a multifactorial condition, the occurrence of which can be attributed to various reasons. Among the main etiological factors, developmental disorders of the foot in childhood, hereditary predisposition, injuries, excess weight, and prolonged improper loading on the legs are highlighted. Other factors that contribute to the development of flatfoot may include shortening of the ligaments and tendons of the foot, anomalies in the development of the joints and muscles of the lower limbs, diseases of the musculoskeletal system and joints.
Understanding the etiology of flatfoot not only helps in determining treatment approaches but also provides effective prevention of this condition. Given the variety of factors influencing the development of flatfoot, it is important to conduct a comprehensive medical examination to identify the underlying cause in each patient, which will allow the appointment of the most effective treatment and prevent the progression of this pathological condition.
- Foot development disorders in childhood: improper formation of the foot during its active growth can lead to flatfoot.
- Hereditary predisposition: genetic factors can increase the likelihood of developing flatfoot in the family.
- Injuries: injuries to the foot, as well as prolonged loads and overloads, can contribute to the development of flatfoot.
- Excess weight: extra weight creates additional pressure on the foot, which can cause deformation and the development of flatfoot.
- Long-term improper loading on the legs: standing work, wearing uncomfortable shoes, or improper weight distribution while walking can cause foot deformities and lead to flatfoot.
The clinical picture of flatfoot
In flatfoot, the clinical picture usually includes various symptoms such as pain when walking, leg fatigue, swelling, and inflammation of the joints, especially in the area of the foot and ankle. Patients may also experience pain in their legs, back, and knees due to foot deformation and poor posture.
In addition, flatfoot can lead to restricted movement in the ankle joints, increased sensitivity of the foot to fatigue, as well as the development of calluses and corns. If the above symptoms are present, it is important to consult a specialist for diagnosis and to determine the optimal treatment plan.
- Pain when walking: Patients with flat feet often experience discomfort and pain in the area of the foot and ankle during movement.
- Leg fatigue: Due to improper weight distribution on the foot with flat feet, the legs tire more quickly when walking and standing.
- Swelling and inflammation: Flat feet can cause swelling and inflammation of the joints, leading to pain and limited movement.
- Pain in legs, back, and knees: Deformation of the feet in flat feet can cause pain in various parts of the body due to poor posture and uneven load.
- Limited movement: Flat feet can lead to reduced mobility of the ankle joints, making regular movements difficult.
Expert opinion on methods of treating flatfoot
Experts in the field of flatfoot usually emphasize the importance of an individualized approach to treating this condition. They recommend a combined approach that includes conservative methods, such as physical therapy, wearing orthopedic shoes, orthoses, and insoles, as well as surgical intervention in cases where conservative treatment does not yield the desired results or in the presence of complications.
Additionally, experts stress the importance of regular monitoring of patients with flatfoot, especially in childhood, to timely adjust treatment and prevent disease progression. They also highlight recommendations for lifestyle changes, including appropriate physical activity, weight control, and avoiding excessive strain on the feet.

Methods for diagnosing flatfoot
To diagnose flat feet, a comprehensive clinical examination is used, which includes an examination by an orthopedic doctor and the performance of X-ray imaging of the foot in two projections. The procedure may involve a visual assessment of the foot’s shape, an analysis of walking, determining the architecture of the foot, as well as measuring the angles of deformation. Additional methods, such as magnetic resonance imaging (MRI) or computed tomography (CT), may be used for a more detailed study of the structures of the foot and joints.
The diagnosis of flat feet plays a key role in determining the degree of foot deformation and allows for the selection of an optimal treatment plan. In the case of flat feet being identified, it is important to begin treatment and prevention of disease progression in a timely manner to prevent possible complications in the future.
- Clinical examination: The doctor conducts a visual and tactile examination of the foot to determine the degree of deformation and architecture.
- X-ray of the foot: Allows for images of the foot in two projections for detailed analysis of anatomical structures and deformation angles.
- Measurement of deformation angles: An important parameter that is assessed as part of the diagnosis to evaluate the degree of flatfoot.
- Gait analysis: A method for evaluating stride, foot positioning, and overall walking mechanics to identify the peculiarities of foot movements in flatfoot.
- Additional methods: MRI and CT may be used for more detailed study of the structures of the foot and joints.
Methods of treating flatfoot
As a rule, the effectiveness of flatfoot treatment directly depends on timely medical assistance and adherence to all doctors’ recommendations. An individualized approach to each patient, as well as a combination of conservative and surgical methods, helps achieve the best results and improve the quality of life for people suffering from flatfoot.
- Orthopedic insoles and footwear: An important method for treating flatfoot is the use of orthopedic insoles, which help support the longitudinal and transverse arches of the foot, as well as properly distribute the load while walking.
- Physical therapy and exercises: Systematic exercises to strengthen the muscles of the feet and calves contribute to the improvement of foot structure, increase its mobility, and reduce pain sensations.
- Medication treatment: Some patients may be prescribed medications to relieve pain, anti-inflammatory drugs for inflammatory processes, as well as vitamins and minerals to maintain the health of the musculoskeletal system.
- Sururgical intervention: In cases where conservative methods do not lead to an improvement in condition or in the presence of significant foot deformations, surgical treatment may be recommended, such as deformity correction, arthrodesis, or implantation of articulating prostheses.
- Preventive measures: An important part of treating flatfoot is prevention, which includes proper shoe selection, maintaining optimal weight, regular physical exercise, and regular visits to the doctor for monitoring and timely detection of possible complications.
Measures for the prevention of flatfoot
Effective prevention of flat feet also includes regular visits to a doctor to monitor the condition of the feet and identify any early signs of deformity. Timely measures to strengthen the foot muscles and follow the specialist’s recommendations can help prevent the development of this condition and maintain the health of the musculoskeletal system for many years.
- Regular exercises for strengthening foot muscles: Performing special exercises for the development of the foot and calf muscles helps improve arch support and prevent flat feet.
- Control of load on the legs: It is important to avoid overworking the feet and to properly distribute the load while walking or standing to prevent foot deformation.
- Choosing footwear with good foot support: Wearing comfortable shoes with good cushioning and support can reduce the risk of developing flat feet and soften the load on the feet.
- Maintaining normal body weight: Excess weight increases the load on the joints and can contribute to the development of flat feet, so maintaining a healthy weight is essential for disease prevention.
- Proper distribution of physical activity: It is important to diversify types of physical exercises, considering their impact on the feet and joints, to prevent possible traumatic loads and foot deformities.
Fascinating aspects of flatfoot
Moreover, flatfoot is a good example of a condition that can be successfully controlled and treated provided there is timely consultation with specialists and adherence to recommendations. The process of studying and treating flatfoot not only contributes to improving the quality of life of patients but also opens up new prospects for the development of diagnostic and therapeutic methods for this condition.