Polycystic kidney disease: three methods of diagnosis and modern treatment options
- Basics of polycystic kidney disease: understanding the disease
- Genetic factors, possible causes of polycystic kidney disease
- How kidney polycystosis manifests: main symptoms and signs
- Expert opinion on the treatment methods for polycystic kidney disease
- Examination in case of suspicion of polycystic kidney disease
- Methods for treating polycystic kidney disease
- Measures to prevent polycystic kidney disease
- Unusual features of kidney polycystosis
- FAQ
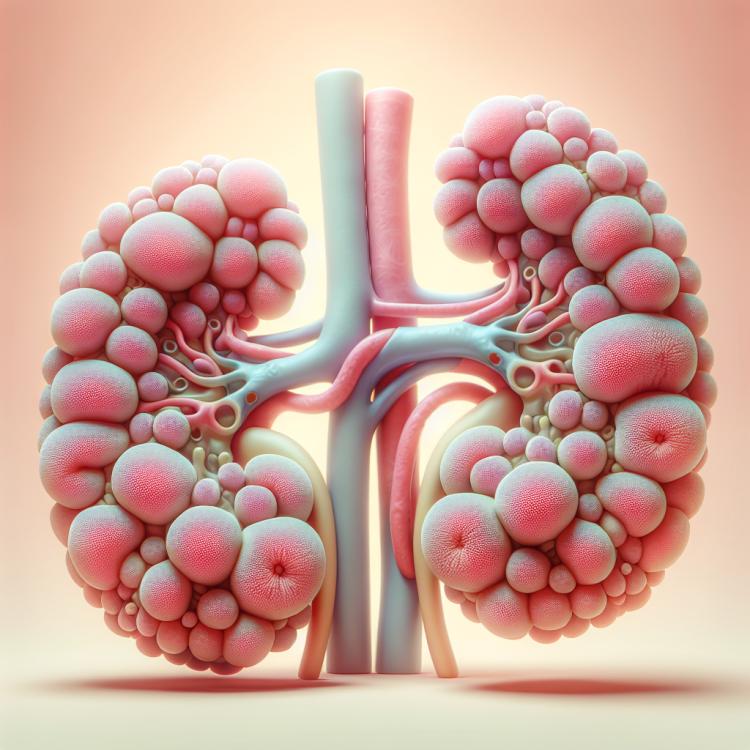
Basics of polycystic kidney disease: understanding the disease
Polycystic kidney disease is a genetic disorder characterized by the formation of multiple cystic formations in the kidney tissue. It can lead to a gradual increase in kidney size, impairment of their functions, and the development of chronic kidney failure. Polycystic kidney disease is often inherited in an autosomal dominant manner and can manifest with various clinical symptoms such as hypertension, hematuria, and pain in the kidney area.
Genetic factors, possible causes of polycystic kidney disease
Polycystic kidney disease is a genetic disorder characterized by the formation of cystic formations in renal tissue. The main genetic mechanisms provoking the development of polycystic kidney disease are mutations in the PKD1 and PKD2 genes, which are responsible for encoding the proteins polycystin-1 and 2, respectively. These mutations lead to the disruption of normal development of renal tubular cells and the formation of cysts, which ultimately results in kidney damage and the progression of the disease. Due to genetic changes in renal tissue, multiple cysts form, which over time lead to a deterioration in kidney function, possible development of kidney failure, and other complications.
- Mutations in genes PKD1 and PKD2: Mutations in these genes, which encode the proteins polycystin-1 and 2 respectively, are considered the main genetic causes of polycystic kidney disease.
- Autosomal dominant inheritance: Polycystic kidney disease is transmitted according to the principle of autosomal dominant inheritance, where a mutation from one parent is sufficient for the development of the disease.
- Somatic mutations: Some cases of polycystic kidney disease may be caused by somatic mutations occurring in kidney tissue cells spontaneously or as a result of environmental factors.
- Disruption of kidney tubule development: Genetic factors can lead to the disruption of normal kidney tubule development, which contributes to the formation of cysts and the development of polycystic disease.
- Multiple modifier genes: In addition to the PKD1 and PKD2 genes, many other genetic factors have been identified that influence the development of polycystic kidney disease and are involved in regulating processes of cell growth and division in kidney tissue.
How kidney polycystosis manifests: main symptoms and signs
Polycystic kidney disease can often manifest asymptomatically in the early stages of the disease. However, as the size of the cysts increases and kidney function deteriorates, symptoms may become noticeable. The main manifestations of polycystic kidney disease include lower back pain, blood in the urine, increased blood pressure, feelings of fatigue and weakness, swelling, and changes in urination. Patients may also exhibit increased abdominal volume due to enlarged kidneys and other signs related to impaired kidney function.
- Lower back pain: pain may occur due to the enlargement of the kidneys and stretching of the capsules.
- Blood in urine: the presence of blood in the urine, or hematuria, can be one of the first signs of kidney pathology.
- Elevated blood pressure: many patients with polycystic kidney disease have hypertension, which may be related to impaired kidney function.
- Fatigue and weakness: patients often complain of general weakness and physical fatigue.
- Swelling and abdominal distension: due to impaired kidney function, swelling may develop in various areas of the body, including the abdominal cavity.
Expert opinion on the treatment methods for polycystic kidney disease
Experts in nephrology and urology draw attention to significant advancements in the treatment methods for polycystic kidney disease. Among the main approaches to therapy, most specialists highlight medication treatment to reduce symptoms, control blood pressure, and maintain kidney function. Experts also note the importance of surgical methods, including the drainage of cysts, laparoscopic removal of part of kidney tissue, as well as kidney transplantation when necessary. In recent years, new approaches have been actively researched, such as gene therapy and the use of innovative drugs, which provide greater hope for more effective treatment of polycystic kidney disease in the future.

Examination in case of suspicion of polycystic kidney disease
In case of suspicion of polycystic kidney disease, important diagnostic methods include performing an ultrasound examination of the kidneys, which allows for the detection of cysts in the kidney tissue. CT and MRI of the kidneys can also be used for a more detailed study of the kidney structure and identification of cysts. Blood tests for creatinine levels and urine tests for the presence of blood and protein help assess kidney function and identify possible complications. Additionally, in the presence of a family history of the disease, genetic testing may help identify the presence of genetic mutations associated with polycystic kidney disease.
- Ultrasound examination of the kidneys: the method of choice for detecting cystic formations in kidney tissue.
- Computed tomography (CT) or magnetic resonance imaging (MRI) of the kidneys: help obtain more detailed information about the structure of the kidneys and detect cysts.
- Blood tests for creatinine levels: an indicator of kidney function, which may be elevated in case of their damage.
- Urine analysis for blood and protein content: helps assess kidney function and detect possible complications.
- Genetic testing: may be aimed at identifying the presence of genetic mutations leading to the development of polycystic kidney disease.
Methods for treating polycystic kidney disease
- Blood pressure control: The use of ACE inhibitors and angiotensin II receptor blockers may help manage blood pressure in patients with polycystic kidney disease.
- Pain management: Analgesics may be recommended to reduce pain associated with polycystic kidney disease.
- Dietary recommendations: Following a diet low in sodium, protein, and phosphorus may be beneficial for patients with polycystic kidney disease to manage symptoms and maintain kidney health.
- Monitoring kidney function: Regular assessments to evaluate kidney function and serum creatinine levels may aid in the early detection of complications and adjustment of treatment.
- Supportive therapy: Some patients may require supportive therapy, including dialysis or kidney transplantation in the event of kidney failure.
Measures to prevent polycystic kidney disease
- Regular medical monitoring: It is important to regularly visit a doctor for screening and monitoring kidney health, especially with a family history of polycystic kidney disease.
- Blood pressure control: Maintaining stable blood pressure helps reduce the burden on the kidneys and lowers the risk of complications.
- Healthy lifestyle: Regular physical exercise, a balanced diet, and adequate water intake contribute to maintaining kidney health.
- Patient education: Patients should be aware of the early signs of polycystic kidney disease and the importance of regular medical check-ups.
- Psychosocial support: Support for patients from specialized services helps cope with emotional stress and improves overall well-being.