Endometrial polyp: causes, symptoms, and treatment methods
- Main aspects of endometrial polyps
- Etiology of endometrial polyp
- Clinical picture of endometrial polyp
- Medical opinion on the therapy of endometrial polyp
- Methods for diagnosing endometrial polyps
- Approaches to the treatment of endometrial polyps
- Measures for the prevention of endometrial polyps
- Amazing facts about endometrial polyps
- FAQ
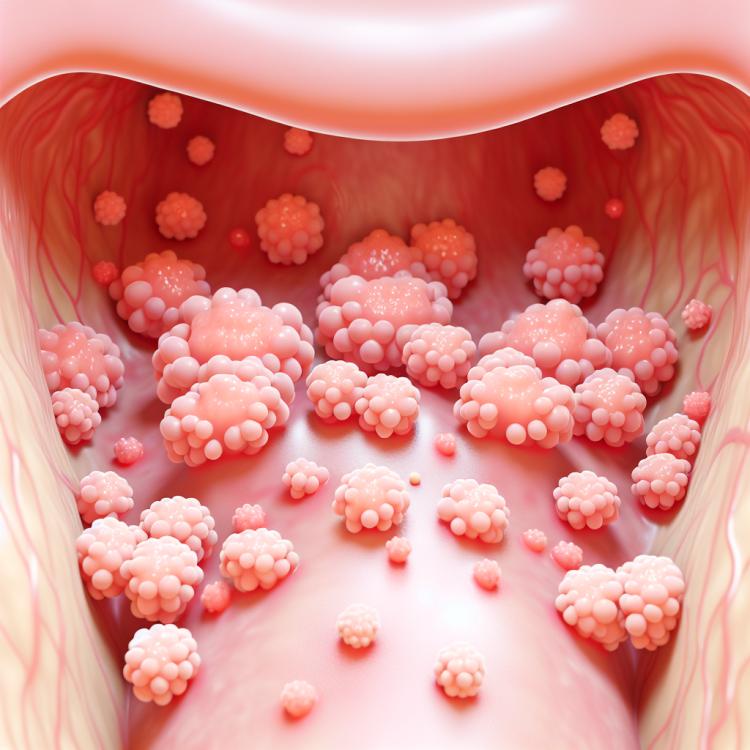
Main aspects of endometrial polyps
The endometrial polyp is a benign tumor-like formation that arises from the mucous membrane of the uterus – the endometrium. The main symptom of an endometrial polyp is irregular or heavy menstrual bleeding, which can lead to anemia and pain in the lower abdomen. The diagnosis of an endometrial polyp includes hysteroscopy, ultrasound examination, and biopsy. Treatment of an endometrial polyp may include observation, hormonal therapy, or surgical removal of the polyp, especially in cases of bleeding, infertility, or suspicion of malignant transformation.
Etiology of endometrial polyp
Endometrial polyps are benign formations that can occur due to various reasons. One of the main factors contributing to the development of polyps is hormonal imbalances, including the imbalance of estrogens and progesterone. Elevated levels of estrogens are one of the common causes for the formation of endometrial polyps, as they promote the proliferation of uterine epithelium.
In addition to hormonal factors, the occurrence of endometrial polyps may be associated with other aspects, such as inflammatory processes in the uterus, disturbances in blood flow, or trauma to the endometrium. Furthermore, genetic predisposition also plays a role in the appearance of endometrial polyps, although the exact mechanism of influence of genetic factors requires further study.
- Hormonal imbalances: Possible causes of endometrial polyps include hormonal dysregulation, such as elevated estrogen levels, which can contribute to the proliferation of the uterine epithelium.
- Inflammatory processes: Chronic inflammation in the endometrial area can promote the formation of polyps.
- Endometrial trauma: Mechanical damage to the uterus, including surgeries or procedures such as scraping, can lead to the development of polyps.
- Genetic predisposition: Hereditary factors may play a role in the occurrence of endometrial polyps, although the mechanism of influence requires further study.
- Medication effects: Certain medications or hormone therapy can cause changes in the endometrium, contributing to the formation of polyps.
Clinical picture of endometrial polyp
The endometrial polyp can manifest various clinical symptoms, including abnormal menstruation, bleeding outside the menstrual cycle, painful periods, dysmenorrhea, as well as possible problems with conception and carrying a pregnancy. Individual patients may also experience lower abdominal pain, unusual vaginal discharge, or general weakness and fatigue.
It is important to consider that the symptoms of an endometrial polyp may vary depending on the size of the polyp, its location, and the individual characteristics of the patient. Diagnosing this condition requires a careful medical examination, the use of specialized diagnostic methods, and subsequent treatment aimed at improving the patient’s condition.
- Abnormal menstruation: an endometrial polyp can lead to changes in regular menstrual cycles, such as heavy or irregular periods.
- Bleeding outside the menstrual cycle: some women with an endometrial polyp may experience bleeding between periods or after sexual intercourse.
- Painful periods: the presence of an endometrial polyp can intensify pain during menstruation for some patients.
- Dysmenorrhea: women with an endometrial polyp may also encounter menstrual function disorders caused by endocrine system disruptions.
- Conception and pregnancy issues: some women with an endometrial polyp may have difficulties with conception or successfully carrying a pregnancy to term.
Medical opinion on the therapy of endometrial polyp
Experts in the field of gynecology and obstetrics typically recommend an individualized approach to the treatment of endometrial polyps. Determining the optimal treatment strategy may involve various methods, such as hormone therapy, hysteroscopic removal of polyps, or even surgical intervention. The decision on choosing a specific method depends on many factors, including the size and number of polyps, clinical symptoms, as well as the patient’s wishes and plans regarding pregnancy.
It is important to note that the treatment of endometrial polyps should be conducted under the supervision of qualified specialists to ensure optimal outcomes and minimize the risks of complications. Consultation with a doctor will help determine the most appropriate treatment plan, taking into account the individual characteristics of each case.

Methods for diagnosing endometrial polyps
For the diagnosis of endometrial polyps, various examination methods are used, including ultrasound, magnetic resonance imaging (MRI), and computed tomography (CT), which allow for the visualization of the uterus structure and the detection of polyps. Hysteroscopy is an endoscopic examination that allows direct visualization of polyps inside the uterus and also enables biopsy or polypectomy during the same procedure.
Additionally, the diagnosis may include a complete blood count and screening for infections or hormonal disorders. The accurate establishment of an endometrial polyp diagnosis plays an important role in prescribing effective treatment and preventing possible complications.
- Ultrasound examination: this method allows obtaining high-resolution images of the uterus’s structure and identifying the presence of polyps.
- Magnetic resonance imaging (MRI): performing an MRI can be useful for confirming the presence of polyps and assessing their characteristics.
- Computed tomography (CT): this examination can also help visualize polyps and supplement data about their location.
- Hysteroscopy: an endoscopic examination that allows visualization of polyps inside the uterus and conducting a biopsy if necessary.
- Blood tests and examination for hormonal disorders: a complete blood count and additional studies can be important for comprehensive diagnosis of endometrial polyps and identifying specific features of the patient.
Approaches to the treatment of endometrial polyps
After a successful endometrial polyp removal procedure, it is important to conduct regular monitoring of the patient to track the effectiveness of the treatment and prevent recurrences. The optimal approach to treating endometrial polyps should be individualized and based on agreement with the patient, taking into account her physiological and psychological characteristics.
-
– **Conservative treatment**: One approach involves the use of hormone therapy aimed at eliminating hormonal imbalances that may contribute to the formation of polyps. This may include the use of progesterone or combined oral contraceptives to suppress the growth of polyps.
– **Surgical intervention**: Surgical removal of the endometrial polyp is usually performed using hysteroscopy. This minimally invasive method allows the procedure to be conducted under video endoscopy control, enabling precise visualization and removal of polyps while minimizing the risk of damaging surrounding tissues.
– **Laser therapy**: The use of laser therapy for the removal of endometrial polyps is becoming an increasingly common method. Laser polypectomy provides precise removal of polyps with minimal damage to surrounding tissues.
– **Regular monitoring and follow-up**: After treatment, it is important to conduct regular monitoring of the patient’s condition. This will allow for the timely detection of potential recurrences and to control the effectiveness of the therapy performed.
– **Individualized approach**: Each case of endometrial polyps is unique, so it is important to approach treatment individually, taking into account the patient’s characteristics, desires, and treatment goals.
Measures for the prevention of endometrial polyps
Additionally, maintaining a healthy lifestyle, including a balanced diet, physical exercise, and avoiding harmful habits like smoking, also plays a role in the prevention of endometrial polyps. In the case of identifying predisposing factors, such as hormonal disorders or heredity, consulting with a doctor can help develop individual preventive measures to maintain endometrial health and prevent possible complications.
- Regular visits to the gynecologist: conducting screening examinations, such as ultrasound and hysteroscopy, helps in the timely detection and monitoring of endometrial polyps.
- Monitoring hormonal balance: properly selected hormone therapy helps regulate the hormonal background and reduce the risk of developing polyps.
- Healthy lifestyle: a balanced diet, regular physical activity, and the rejection of harmful habits, including smoking, have a positive effect on the condition of the endometrium.
- Monitoring predisposing factors: in the presence of hormonal disorders or hereditary factors, it is important to consult a doctor to develop individual preventive measures.
- Self-referral to a specialist: in case of unusual symptoms or changes in the menstrual cycle, it is important to consult a doctor to assess the condition of the endometrium and prevent possible complications.
Amazing facts about endometrial polyps
As one of the most common intrauterine formations in women, endometrial polyps remain the subject of active scientific research in the field of gynecology and obstetrics. An interesting fact is that modern diagnostic and treatment methods allow for improving the prognosis for patients with endometrial polyps, reducing the risk of complications and maintaining women’s health at an appropriate level.