Endometrial polyp in the uterus: diagnosis, consequences, and removal methods
- Understanding Endometrial Polyps: Symptoms, Diagnosis, and Treatment
- Etiology of Endometrial Polyp: Risk Factors and Pathogenesis
- Clinical picture of an endometrial polyp: what catches the attention?
- Expert opinion on the methods of treating endometrial polyps
- Methods for diagnosing endometrial polyps in the uterus
- Methods of treating endometrial polyps in the uterus
- Measures for the prevention of endometrial polyps in the uterus
- Amazing aspects of endometrial polyps in the uterus
- FAQ
Understanding Endometrial Polyps: Symptoms, Diagnosis, and Treatment
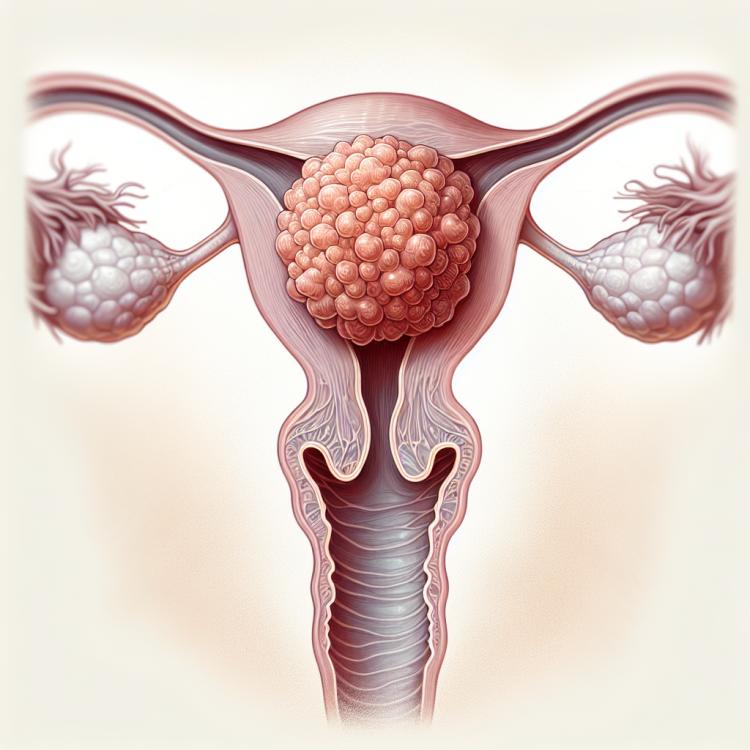
An endometrial polyp is a benign formation of the inner layer of the uterus, often manifesting through abnormal bleeding in women of reproductive age. Symptoms may include menstrual disturbances, bleeding outside the menstrual cycle, or infertility.
To diagnose a polyp, ultrasound examination, hysteroscopy, or hysterosalpingography are used. Treatment usually involves the surgical removal of the polyp, which can improve clinical symptoms and promote the restoration of reproductive function in women with a diagnosed endometrial polyp.
Etiology of Endometrial Polyp: Risk Factors and Pathogenesis
Endometrial polyps are hyperplastic formations of the inner layer of the uterus – the endometrium. The pathogenesis of endometrial polyps is associated with hormonal changes, including hyperestrogenism and progesterone deficiency, which contribute to the inadequate growth of endometrial cells. Risk factors for the development of polyps include hormonal imbalances, obesity, endometrial hyperplasia, and endocrine disorders.
The main causes of endometrial polyps in the uterus are linked to hormonal factors, as well as inflammatory processes and genetic mutations. It is not uncommon for polyps to occur against a background of proliferative changes in the endometrium or as a result of excessive accumulation of glycosaminoglycans. It is important to consider that understanding the causes and pathogenesis of endometrial polyps in the uterus is key to successful diagnosis, treatment, and prevention of recurrences of this condition.
- Hormonal imbalances: Hyperestrogenism and a lack of progesterone contribute to inadequate growth of endometrial cells, which can lead to the formation of polyps.
- Obesity: Excess weight is associated with hormonal changes that may contribute to the development of polyps in the endometrium.
- Endometrial hyperplasia: Proliferative changes in the endometrium can lead to the formation of polyps.
- Endocrine disorders: Disorders in the endocrine system may be associated with the formation of endometrial polyps in the uterus.
- Genetic mutations: Some genetic abnormalities may lead to an increased risk of developing polyps in the endometrium.
Clinical picture of an endometrial polyp: what catches the attention?
Endometrial polyps in the uterus can manifest a wide range of symptoms, including abnormal menstruation such as heavy or prolonged menstrual bleeding, as well as intermenstrual bleeding. Some patients may report specific complaints of bloody discharge after intercourse or physical activity. There may also be ailments in the form of lower abdominal or pelvic pain, especially during menstruation.
Patients with endometrial polyps may also experience other symptoms, including infertility, which may be related to impaired embryo implantation due to the presence of the polyp. In some cases, endometrial polyps in the uterus can remain asymptomatic and are discovered incidentally during a gynecological examination or ultrasound. Nevertheless, if the aforementioned clinical manifestations are present, it is advisable to consult a doctor for further examination and treatment recommendations.
- Abnormal menstruation: heavy or prolonged menstrual bleeding may be a sign of an endometrial polyp.
- Intermenstrual bleeding: the appearance of bleeding between menstruations may indicate the presence of a polyp in the uterus.
- Bloodstained discharge: after sexual intercourse or physical exertion may be one of the symptoms of an endometrial polyp in the uterus.
- Pain sensations: pain in the lower abdomen or pelvic area, especially during menstruation, may be associated with endometrial polyps.
- Infertility: the presence of an endometrial polyp may negatively impact the embryo implantation process and lead to infertility.
Expert opinion on the methods of treating endometrial polyps
Experts in the field of gynecology express their views on various methods of treating endometrial polyps in the uterus, emphasizing the importance of an individualized approach to each clinical case. The main methods for treating endometrial polyps include conservative approaches, such as the use of hormone therapy to address hormonal imbalances that contribute to polyp growth. Additionally, hysteroscopy may be used to remove polyps — a minimally invasive surgical procedure with high effectiveness and low risk of complications.
Experts emphasize the importance of timely detection of endometrial polyps and the appointment of appropriate treatment to prevent possible complications, such as infertility or recurrences. They also note that patients diagnosed with endometrial polyps require regular monitoring and management of their condition, which will help prevent the recurrence of polyps and ensure optimal conditions for maintaining reproductive health.

Methods for diagnosing endometrial polyps in the uterus
Diagnosis of endometrial polyps in the uterus includes various examination methods, starting with a general analysis of the patient’s symptoms and complaints. The main diagnostic method is a gynecological examination, which allows for the detection of changes in the endometrium and, if necessary, the performance of colposcopy for a detailed study of the cervix area. Ultrasound examination of the pelvic organs is used for a more accurate determination of the size and shape of the polyp.
Additional diagnostic methods may include hysteroscopy – a visual examination of the uterine cavity using a hysteroscope, as well as endometrial biopsy for histological examination of the formation. Multislice computed tomography (MSCT) and magnetic resonance imaging (MRI) may also be used for additional assessment of the polyp, especially in cases where there is suspicion of malignant transformation. The comprehensive use of various diagnostic methods allows for the determination of the nature and size of the polyp, the selection of the optimal treatment method, and the provision of the most effective treatment for the patient.
- Gynecological examination: the initial stage of diagnosis, allowing to identify changes in the endometrium and determine possible compromising factors.
- Ultrasound examination: used to determine the size and shape of the polyp, as well as its structural features in the uterine cavity.
- Hysteroscopy: performing a visual examination of the uterine cavity using a hysteroscope for accurate determination of the characteristics of the polyp.
- Endometrial biopsy: a procedure that allows taking a tissue sample from the endometrium for subsequent histological examination for pathological changes.
- Multislice computed tomography (MSCT) and magnetic resonance imaging (MRI): additional diagnostic methods used to confirm the diagnosis and assess the polyp in various projections.
Methods of treating endometrial polyps in the uterus
Hormone therapy, which includes the use of progesterone or combined oral contraceptives, can be used to reduce the size of the polyp and prevent its recurrence. Surgical removal of the polyp is usually performed for larger polyps or in the presence of symptoms such as heavy menstrual bleeding. Hysteroscopic removal of the polyp, with high efficacy and minimal risk of damage to surrounding tissues, is one of the most common treatments for endometrial polyps in the uterus.
- Hormonal therapy: The use of progesterone or combined oral contraceptives may help reduce the size of the polyp and prevent recurrences.
- Surgical removal: In cases of large polyps or the presence of symptoms such as heavy menstrual bleeding, surgical removal may be required.
- Hysteroscopy with removal: This method, where the polyp is removed using a hysteroscope, is an effective and safe treatment option.
- Minimally invasive procedures: Methods such as radiofrequency coagulation or cryoablation may be possible to remove endometrial polyps in the uterus with minimal impact on surrounding tissues.
- Pathological biopsy: After polyp removal, a pathological biopsy may be performed for histological examination and clarification of the diagnosis.
Measures for the prevention of endometrial polyps in the uterus
Maintaining a healthy lifestyle, including a balanced diet, regular physical activity, and avoiding harmful habits such as smoking, also helps prevent the occurrence of endometrial polyps. An important aspect of prevention is also timely treatment of inflammatory processes in the pelvic organs and monitoring the condition of the endocrine system. Regularly following the doctor’s recommendations for health monitoring and seeking medical assistance promptly in case of symptoms can help minimize the risk of developing endometrial polyps in the uterus.
- Regular visits to the gynecologist: Conducting regular preventive examinations with gynecological assessments can help identify potential problems at an early stage and prevent the development of polyps.
- Monitoring hormonal balance: Establishing and maintaining a normal hormonal background helps reduce the risk of endometrial hyperplasia, which can prevent the appearance of polyps.
- Healthy lifestyle: Regular physical exercise, a balanced diet, and avoiding smoking and alcohol contribute to overall health improvement and reduce the risk of diseases, including endometrial polyps.
- Maintaining optimal weight: Being overweight can be a risk factor for hormonal disorders, which may contribute to the development of pathological changes in the endometrium.
- Treatment of inflammatory processes: Timely medical assistance for inflammation in the pelvic organs and their effective treatment helps prevent potential complications, including the formation of endometrial polyps.
Amazing aspects of endometrial polyps in the uterus
Additionally, an interesting aspect of the endometrial polyp is its ability to recur. After surgical removal of the polyp, there is a possibility of this neoplasm re-forming, especially in the case of ongoing hormonal imbalances or other provocative factors. This circumstance emphasizes the importance of postoperative monitoring and maintaining hormonal stability in patients diagnosed with endometrial polyps in the uterus.