Post-infarction cardiomyopathy: main aspects and treatment methods
- Analysis of the term: post-infarction cardiosclerosis
- Possible mechanisms of post-infarction cardiosclerosis development
- The clinical picture of post-infarction cardiosclerosis
- Expert opinions on the treatment of post-infarction cardiosclerosis
- Methods for diagnosing post-infarction cardiosclerosis
- Strategies for the treatment of post-infarction cardiosclerosis
- Measures for the prevention of post-infarction cardiosclerosis
- Amazing aspects of post-infarction cardiosclerosis
- FAQ
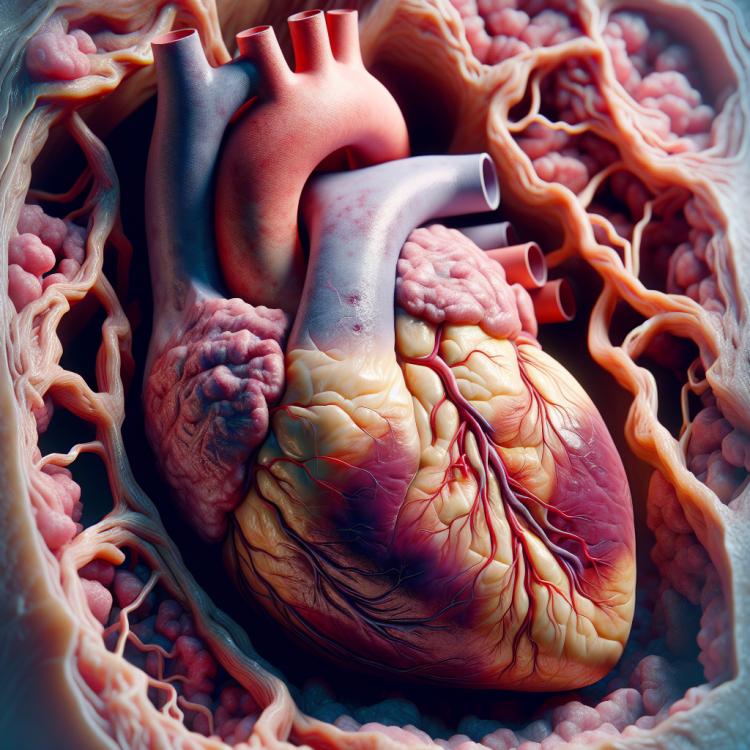
Analysis of the term: post-infarction cardiosclerosis
Post-infarction cardiosclerosis is a pathological condition of the heart tissue that occurs after a myocardial infarction. As a result of the infarction, a necrotic area of tissue forms, which undergoes remodeling during the healing process. This leads to the appearance of a scar – altered tissue that has poor contractile function and worsens heart performance. Post-infarction cardiosclerosis is often accompanied by arrhythmias and structural changes in the heart, which increase the risk of cardiovascular complications. An important aspect of treating this condition is controlling risk factors (blood pressure, cholesterol, blood sugar) and prescribing medication therapy to prevent the progression of post-infarction cardiosclerosis and reduce the risk of recurrent cardiovascular events.
Possible mechanisms of post-infarction cardiosclerosis development
Post-infarction cardiosclerosis can develop due to damage to the myocardium as a result of a myocardial infarction, which leads to the replacement of necrotic tissue with connective tissue. This process can lead to changes in the structure and function of the heart, causing the occurrence of cardiosclerosis. In addition, inflammatory processes in the post-infarction period can also contribute to the development of cardiosclerosis.
- Myocardial damage: myocardial necrosis caused by a heart attack can lead to the replacement of necrotic tissue with connective tissue.
- Inflammatory processes: inflammation occurring after a heart attack can contribute to the development of cardiac sclerosis.
- Remodeling of heart structure: changes in the structure of the myocardium after a heart attack can lead to further development of cardiac sclerosis.
- Ischemia and hypoxia: a lack of oxygen and nutrients in the heart tissue can contribute to the development of cardiac sclerosis.
- Heart hypertrophy: an increase in heart size in response to increased load can also contribute to the onset of cardiac sclerosis.
The clinical picture of post-infarction cardiosclerosis
The clinical picture of post-infarction cardiosclerosis can manifest with various symptoms, including fatigue, shortness of breath, edema, malaise, a feeling of heaviness in the chest, or even pain, which may be caused by changes in the heart’s structure and function. Patients may also experience heart rhythm disturbances, which can lead to arrhythmias. Diagnosing post-infarction cardiosclerosis is important for the timely initiation of treatment and prevention of complications.
- Fatigue and weakness: patients with post-infarction cardiosclerosis often experience increasing fatigue and weakness, which is related to impairments in cardiac function.
- Shortness of breath: breathing problems, including shortness of breath even at rest, may be one of the symptoms of post-infarction cardiosclerosis due to worsening heart function.
- Edema: fluid retention in the body can cause edema, especially in the legs and ankles, in patients with post-infarction cardiosclerosis.
- Chest pain: patients may sometimes experience pain, discomfort, or pressure in the chest area, caused by changes in heart structure.
- Arrhythmias: changes in heart tissue after myocardial infarction can provoke disturbances in heart rhythm, manifesting as arrhythmias and irregular heart contractions.
Expert opinions on the treatment of post-infarction cardiosclerosis
Experts in the field of cardiology recommend a comprehensive approach to the treatment of post-infarction cardiosclerosis, which includes pharmacological therapy, rehabilitation measures, control and correction of risk factors, as well as surgical methods when necessary. The main goal of treatment is to prevent the progression of cardiosclerosis, improve heart function, reduce the risk of complications, and enhance the quality of life for patients.
Experts emphasize the importance of early initiation of treatment and regular monitoring of the patient’s condition for effective management of post-infarction cardiosclerosis. An individualized approach for each patient, taking into account the specifics of their condition, helps achieve the best treatment outcomes and prevent possible complications.

Methods for diagnosing post-infarction cardiosclerosis
Various methods are used for the diagnosis of post-infarction cardioclerosis, including ECG, echocardiography, cardiac magnetic resonance imaging (MRI), computed tomography (CT), and coronary angiography. ECG allows for the assessment of the electrical activity of the heart and the identification of signs of pathology. Echocardiography can be used to visualize cardiac structures and evaluate heart function. MRI and CT provide detailed images of the heart, which helps identify changes at the cellular level. Coronary angiography allows for the assessment of the condition of the coronary arteries and the identification of the degree of occlusion, which is important for treatment planning.
- Electrocardiography (ECG): ECG is one of the main methods for diagnosing post-infarction cardiosclerosis, allowing for the assessment of the electrical activity of the heart and the identification of changes.
- Echo cardiography: Echocardiography is used to visualize the structures of the heart and assess its function after a myocardial infarction.
- Magnetic resonance imaging (MRI) of the heart: MRI provides detailed images of the heart, helping to identify changes at the cellular level.
- Computed tomography (CT): CT of the heart allows for high-quality imaging of the heart and coronary arteries for more accurate diagnosis of post-infarction conditions.
- Coronary angiography: This invasive method allows for the assessment of the condition of the coronary arteries and the identification of the degree of vessel damage, which is important for determining subsequent treatment strategies.
Strategies for the treatment of post-infarction cardiosclerosis
- Medication therapy: Includes the use of medications to control blood pressure, improve heart function, and prevent cardiac complications.
- Regular monitoring by a specialist: It is important to visit a doctor for assessing heart condition, adjusting treatment, and minimizing the risk of complications.
- Lifestyle changes: Includes a healthy diet, physical exercise, quitting smoking, and moderate alcohol consumption to improve heart condition and overall health.
- Rehabilitation: Programs for physical and psychological rehabilitation help restore health and improve quality of life after a myocardial infarction.
- Surgical methods: In some cases, surgical intervention may be required, such as stenting or coronary artery bypass grafting, to restore normal blood flow to the heart.
Measures for the prevention of post-infarction cardiosclerosis
- Blood pressure control: regular monitoring and maintenance of optimal pressure help prevent further damage to the heart and blood vessels.
- Cholesterol level control: lowering “bad” cholesterol and raising “good” cholesterol helps prevent the formation of plaques in the arteries.
- Quitting smoking: tobacco smoke damages the walls of blood vessels and contributes to the development of atherosclerosis, which increases the risk of post-infarction cardiomyopathy.
- Physical exercise: regular workouts help strengthen the cardiovascular system and reduce the likelihood of heart complications.
- Healthy eating: consuming nutritious foods rich in vitamins, minerals, and antioxidants helps maintain the health of the heart and blood vessels.