Postcholecystectomy syndrome: diagnosis and treatment methods.
- Understanding Postcholecystectomy Syndrome: Key Facts.
- Expert study of the causes of Postcholecystectomy Syndrome development
- Recognition of symptoms of Postcholecystectomy syndrome
- The doctors’ perspective on effective treatment methods for postcholecystectomy syndrome.
- Definition of Postcholecystectomy Syndrome through Diagnostic Methods
- Effective strategies for treating Postcholecystectomy Syndrome
- The importance of preventing Postcholecystectomy Syndrome
- Funny aspects of Postcholecystectomy syndrome
- FAQ
Understanding Postcholecystectomy Syndrome: Key Facts.
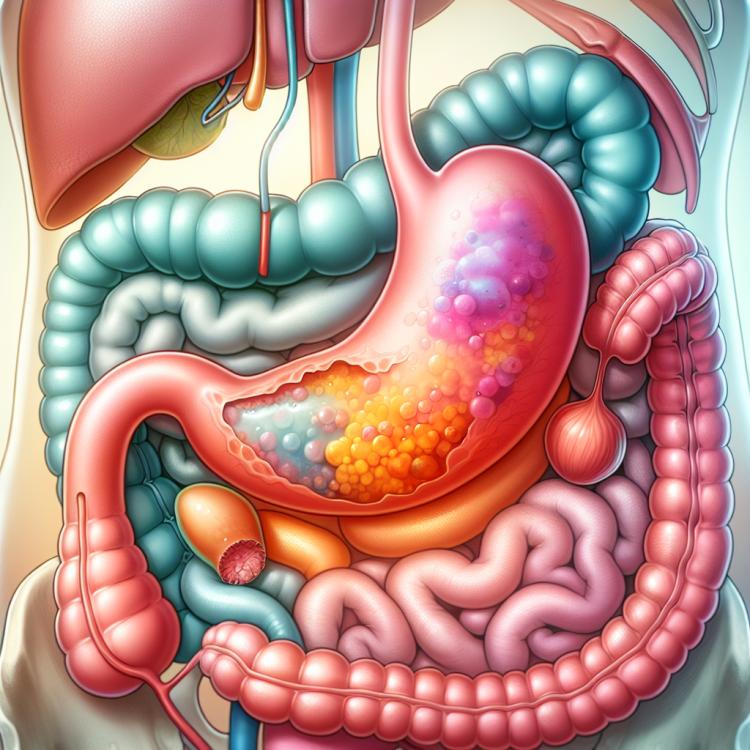
Postcholecystectomy syndrome (PHES) is a complication that can occur after the removal of the gallbladder, cholecystectomy. The main symptoms of PHES are pain in the right upper quadrant, dyspepsia, and diarrhea, which worsen after consuming fatty foods. The mechanism of PHES development remains insufficiently understood; however, it is suggested that changes in the bile ducts and the fermentation of fats may play a role in its pathogenesis. The diagnosis of PHES is based on clinical symptoms but may require laboratory tests and instrumental examinations to rule out other possible causes of the symptoms.
Expert study of the causes of Postcholecystectomy Syndrome development
Postcholecystectomy syndrome (PHES) is a complication that can occur after gallbladder removal. The main causes of its development are disorders of the biliary system, including obstructions of the bile ducts, cholelithiasis, and inflammatory processes. Expert examination of these causes allows for the identification of the mechanisms leading to the development of this syndrome and determining the most effective strategies for treatment and prevention of its complications.
- Gallstone disease: the presence of stones in the gallbladder or bile ducts may contribute to the development of PHES.
- Bile duct obstruction: blockage of the bile ducts for various reasons can lead to the occurrence of the syndrome.
- Inflammatory processes: chronic cholecystitis or other inflammatory diseases of the gallbladder may act as a catalyst for the development of PHES.
- Dysfunction of the gallbladder: dysfunction of the gallbladder, including improper contraction or pathological changes, may be the cause of the syndrome.
- Postoperative complications: improper methods and techniques of cholecystectomy, as well as complications following the surgery, may contribute to the development of PHES.
Recognition of symptoms of Postcholecystectomy syndrome
Postcholecystectomy syndrome manifests with various symptoms, including pain in the right upper quadrant of the abdomen, dyspepsia, nausea and vomiting, as well as bile regurgitation. Patients may also experience discomfort in the abdomen after consuming fatty, spicy, or fried foods, which is due to digestive process disruptions.
Other symptoms of Postcholecystectomy syndrome may include diarrhea, bloating, heartburn, and a feeling of heaviness or discomfort in the epigastric area. It is important to consider that the symptoms may vary for each patient, so for an accurate diagnosis and treatment plan, it is necessary to consult a qualified specialist.
- Pain in the right upper quadrant of the abdomen: often sharp or dull pains in the stomach area can be the first sign of Postcholecystectomy Syndrome.
- Dyspepsia: digestive disturbances such as belching, heartburn, flatulence, and nonspecific pain can be symptoms of this syndrome.
- Nausea and vomiting: feelings of nausea and vomiting, especially after consuming fatty or heavy foods, may indicate the presence of Postcholecystectomy Syndrome.
- Diarrhea: frequent involuntary stools can be one of the manifestations of the syndrome, related to changes in the digestive process.
- Heartburn and bloating: a feeling of bitterness or acidity in the esophagus and abdominal bloating can accompany Postcholecystectomy Syndrome.
The doctors’ perspective on effective treatment methods for postcholecystectomy syndrome.
Experts in the fields of gastroenterology and surgery discuss various treatment methods for Postcholecystectomy Syndrome, including conservative approaches and surgical interventions. According to their opinion, the choice of the optimal treatment method depends on the severity of symptoms, the presence of complications, and the overall condition of the patient.
In acute forms of the syndrome, emergency surgical intervention may be necessary to prevent further complications. However, in cases of chronic processes, specialists usually prefer to start with conservative treatment, which includes diet, medication therapy, and physical exercises. Great importance is also placed on an individualized approach to each patient and modern diagnostic methods to determine the most effective treatment plan.

Definition of Postcholecystectomy Syndrome through Diagnostic Methods
The diagnosis of postcholecystectomy syndrome involves a comprehensive study aimed at identifying the main symptoms and changes characteristic of this condition. Clinical examination, patient history, laboratory, and instrumental methods of investigation play a key role in diagnosing the syndrome. Laboratory analyses of biochemical indicators, such as bilirubin levels, liver enzymes, blood and urine tests for the presence of inflammatory processes, assist in assessing the functional state of the digestive organs.
Instrumental methods, such as ultrasound examination of the abdominal organs, magnetic resonance cholangiography, and endoscopic retrograde cholangiopancreatography, may be used for more precise diagnosis of the condition of the bile ducts and biliary production indicators after cholecystectomy. A comprehensive approach to diagnosis will help identify the causes of symptoms related to postcholecystectomy syndrome and develop an effective treatment plan for each patient.
- Clinical examination of the patient, including the identification of characteristic symptoms of Postcholecystectomy syndrome, such as pain in the right upper quadrant of the abdomen.
- History taking, including information about previous surgeries for gallbladder removal and the presence of cholelithiasis.
- Laboratory tests to assess biochemical indicators, such as levels of bilirubin and liver enzymes.
- Instrumental methods, including ultrasound examination of the abdominal organs to assess the condition of the liver and bile ducts.
- Additional studies, such as magnetic resonance cholangiography and endoscopic retrograde cholangiopancreatography, for more detailed visualization of the bile ducts and assessment of their functions.
Effective strategies for treating Postcholecystectomy Syndrome
In some cases, surgical intervention may be required, for example, in the presence of complications such as biliary hypertension or segmental syndrome. The decision about the necessity and type of surgical treatment is made after a comprehensive examination and assessment of the patient’s condition by a specialist. Effective treatment strategies for postcholecystectomy syndrome aim to improve the patient’s quality of life, reduce symptoms, and prevent complications.
- Diet with limited fatty foods: moderate consumption of fats helps reduce the burden on the digestive system and decrease the risk of exacerbating symptoms.
- Use of choleretic agents: drugs that promote the dilution and excretion of bile can improve the functioning of the gallbladder and bile ducts.
- Control over food intake: regular small meals and avoiding overeating can help reduce the load on the digestive system and minimize discomfort.
- Use of dietary supplements: the use of enzyme preparations or probiotics can aid in improving digestion and alleviating dyspeptic symptoms.
- Individual pharmacotherapy: the prescription of medications under the supervision of a doctor, depending on the clinical picture and patient characteristics, can help manage the symptoms of Postcholecystectomy syndrome.
The importance of preventing Postcholecystectomy Syndrome
Particular attention should be paid to following the doctors’ recommendations after gallbladder removal surgery, including the proper use of medications, adequate nutrition, and regular check-ups for timely detection of possible complications. Adhering to preventive recommendations helps reduce the risk of Postcholecystectomy Syndrome and assists patients in coping with the consequences of gallbladder removal more effectively.
- Adhering to doctors’ recommendations after surgical removal of the gallbladder helps prevent the development of Postcholecystectomy syndrome.
- Limiting the intake of fatty and abundant foods helps reduce the strain on the digestive system and lowers the risk of gallstone formation.
- Rational nutrition with the mandatory inclusion of dietary fibers contributes to the normalization of gastrointestinal function and prevents dysbiosis.
- Consuming an adequate amount of water helps dissolve and eliminate metabolic waste from the body through the urinary tract.
- Regular examinations and consultations with a doctor allow for the early detection of possible changes in the body and timely adjustment of treatment measures.
Funny aspects of Postcholecystectomy syndrome
Interesting facts related to Postcholecystectomy syndrome can reflect unusual aspects of this condition and stimulate further study of its mechanisms of occurrence and treatment. Discussions about various theories of the development of this syndrome may lead to new discoveries and methods of prevention and treatment of this disease.