Post-thrombotic syndrome: features, diagnosis and treatment methods
- Understanding post-thrombotic syndrome
- Risk factors for the development of post-thrombotic syndrome
- The main manifestations of post-thrombotic syndrome
- Expert opinions on the treatment of post-thrombotic syndrome
- Methods for diagnosing post-thrombotic syndrome
- Methods of treating post-thrombotic syndrome
- Methods for the prevention of post-thrombotic syndrome
- Interesting aspects of post-thrombotic syndrome
- FAQ
Understanding post-thrombotic syndrome
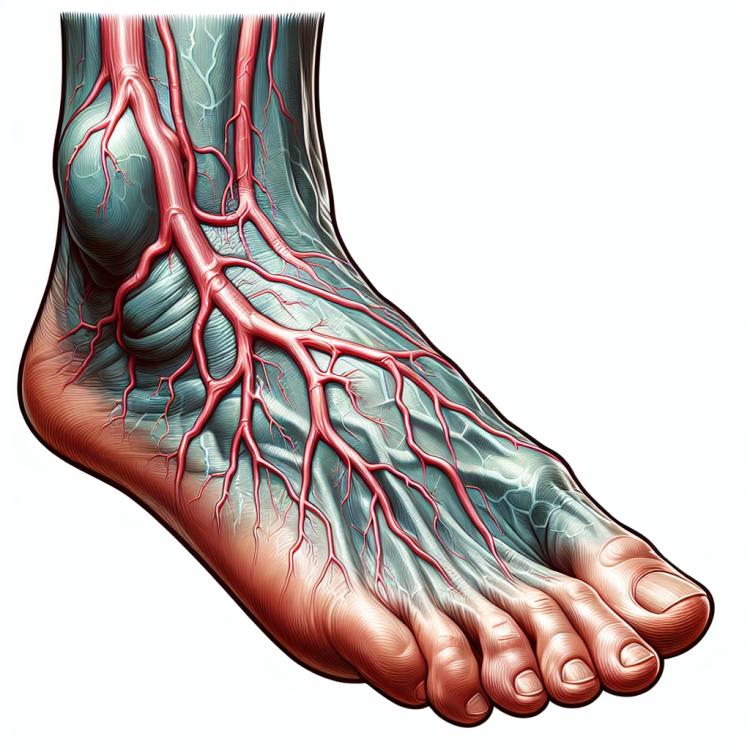
Post-thrombotic syndrome is a complication of venous thromboembolic disease, characterized by inflammation of the venous walls following a previous episode of thrombosis. This condition often leads to chronic changes in the venous system and can manifest as swelling, pain, and a feeling of heaviness in the legs. It is important to detect and treat post-thrombotic syndrome in a timely manner, as it can progress, causing serious complications including ulcers and thromboembolic events.
Risk factors for the development of post-thrombotic syndrome
Risk factors for the development of post-thrombotic syndrome include a history of previous thrombosis or post-thrombotic conditions, hereditary predisposition to thrombosis, prolonged stationary treatment, especially with surgical interventions, prolonged immobility, musculoskeletal disorders that limit physical activity. In addition, risk factors may include obesity, pregnancy, blood system pathologies, age over 40, and a number of other comorbidities. It is important to identify and consider these factors in the diagnosis and implementation of preventive measures to prevent the development of post-thrombotic syndrome.
- Previous cases of thrombosis or post-thrombotic syndrome: A history of thrombosis increases the risk of subsequent cases of thrombosis and post-thrombotic disease.
- Hereditary predisposition to thrombosis: Genetic factors may lead to an increased risk of developing post-thrombotic disease.
- Prolonged inpatient treatment with surgical interventions: Postoperative states may contribute to the formation of clots and the development of post-thrombotic disease.
- Prolonged immobility: Limited physical activity may create optimal conditions for the formation of clots.
- Obesity and overweight: Increased body fat can elevate the load on the venous system and enhance the risk of developing post-thrombotic disease.
The main manifestations of post-thrombotic syndrome
Post-thrombotic syndrome is characterized by various symptoms, including swelling and pain in the area of the affected vessel, skin hyperpigmentation, and signs of chronic venous insufficiency. Patients may also experience a feeling of heaviness, tension, and fatigue in the legs, and sometimes exhibit trophic ulcers, changes in the structure of the skin, and subcutaneous tissue.
In the late stages of the disease, complications such as trophic ulcers or hyperpigmentation may arise. For accurate diagnosis and optimal treatment choice, it is important to consider all characteristic symptoms of post-thrombotic syndrome, as they can vary depending on the degree of venous system damage and individual patient characteristics.
- Swelling and pain: post-thrombotic syndrome is often accompanied by swelling and tenderness in the area of the affected vessel.
- Skin hyperpigmentation: patients with post-thrombotic syndrome often have areas of skin with altered color.
- Feeling of heaviness and fatigue in the legs: patients may complain of a feeling of heaviness, fatigue, and tension in the legs, especially after physical exertion.
- Trophic ulcers: some patients with post-thrombotic syndrome may develop trophic ulcers on the skin of the legs.
- Changes in the structure of the skin and subcutaneous tissue: the disease can lead to changes in the structure of the skin, the appearance of nodules, and thickening in the area of the affected veins.
Expert opinions on the treatment of post-thrombotic syndrome
Experts in the field of medicine recommend a comprehensive approach to the treatment of post-thrombotic syndrome, including conservative methods, surgical intervention, and wearable compression garments. Treatment is usually aimed at reducing inflammation and pain, improving blood circulation, and preventing complications such as trophic ulcers.
The determination of the optimal treatment method depends on the severity of the disease, the individual characteristics of the patient, and the presence of complications. Experts evaluate the effectiveness of therapy based on clinical studies, taking into account both the current condition of the patient and the prognosis of long-term outcomes.

Methods for diagnosing post-thrombotic syndrome
For the diagnosis of post-thrombotic syndrome, various methods are used, starting from clinical examination and patient history to functional and instrumental studies. Clinical examination includes analysis of symptoms, inspection of affected areas of the skin, as well as palpation and examination of vessel pulsation.
Instrumental diagnostic methods, such as ultrasound duplex scanning, can aid in determining the presence of clots, the extent of vessel damage, and assessing blood flow. Computed tomography and magnetic resonance angiography can also be used for additional visualization. Accurate and timely diagnosis is a key stage in the examination of patients suspected of having post-thrombotic syndrome.
- Clinical examination: includes the analysis of complaints and symptoms, examination of skin changes, palpation of affected areas, and study of vessel pulsation.
- Ultrasound duplex scanning: allows visualization of the vascular wall, determination of the presence of thrombi, and assessment of the degree of damage to the venous system.
- Computed tomography: can be used for additional diagnosis, providing information about the condition of vessels and tissues in the bedside area.
- Magnetic resonance angiography: provides detailed images of vessels and allows assessment of blood flow in the affected area.
- Laboratory studies: may include blood tests for inflammatory markers and others to identify additional signs of inflammation and thrombosis.
Methods of treating post-thrombotic syndrome
In addition, pharmacological agents such as anticoagulants, anti-inflammatory drugs, and medications that improve microcirculation may be used for the treatment of post-thrombotic syndrome. An individualized approach to the selection of treatment methods and the combination of several therapeutic approaches enable achieving the best results in the treatment of post-thrombotic syndrome.
- Compression therapy: includes the use of compression garments or bandages to improve blood flow in the affected veins and reduce swelling.
- Physical activity: engage in moderate physical exercises and follow recommendations for strengthening muscles and improving venous circulation.
- Pharmacological therapy: includes the use of medications such as anticoagulants to prevent the formation of new blood clots, anti-inflammatory drugs to reduce inflammation, and analgesics to alleviate pain symptoms.
- Surgical intervention: in some cases, surgical treatment may be required, such as surgical removal of a clot or correction of affected veins.
- Diet and lifestyle: important aspects of a healthy lifestyle, including a balanced diet, maintaining a normal weight, avoiding harmful habits, and following doctor’s recommendations.
Methods for the prevention of post-thrombotic syndrome
For patients with a particularly high risk of thrombosis, such as after surgical interventions or with a hereditary predisposition, the use of anticoagulants and other medications for thrombosis prevention may be recommended. Effective prevention of post-thrombotic syndrome is important for maintaining the health of the venous system and preventing complications.
- Physical activity: Regular physical exercises promote better blood flow and reduce the risk of thrombosis.
- Weight management: Maintaining a healthy weight helps prevent unnecessary pressure on the veins and improves blood flow.
- Avoiding prolonged sitting or standing: Regular breaks and changing body positions help prevent blood stagnation and the formation of clots.
- Quitting smoking: Nicotine constricts blood vessels, worsening blood circulation and increasing the risk of thrombosis.
- Using compression garments: Wearing special compression garments helps improve venous circulation and reduce swelling in the limbs.
Interesting aspects of post-thrombotic syndrome
In addition to physical manifestations, post-thrombotic syndrome can significantly affect the quality of life of the patient due to pain, limitations in mobility, and cosmetic defects. Studying this disease highlights the importance of timely intervention and effective treatment to prevent complications and maintain the health of the venous system.