Lumbar spondylosis: causes, symptoms, and treatment methods
- Fundamentals of Understanding Lumbar Spondylosis
- Factors for the onset of lumbar spondylosis
- The clinical picture of lumbar spondylosis
- The specialists’ perspective on the treatment methods for lumbar spondylosis
- Methods for diagnosing lumbar spondylosis
- Methods of treating lumbar spondylosis
- Prevention measures for lumbar spondylosis
- Amazing aspects of lumbar spondylosis
- FAQ
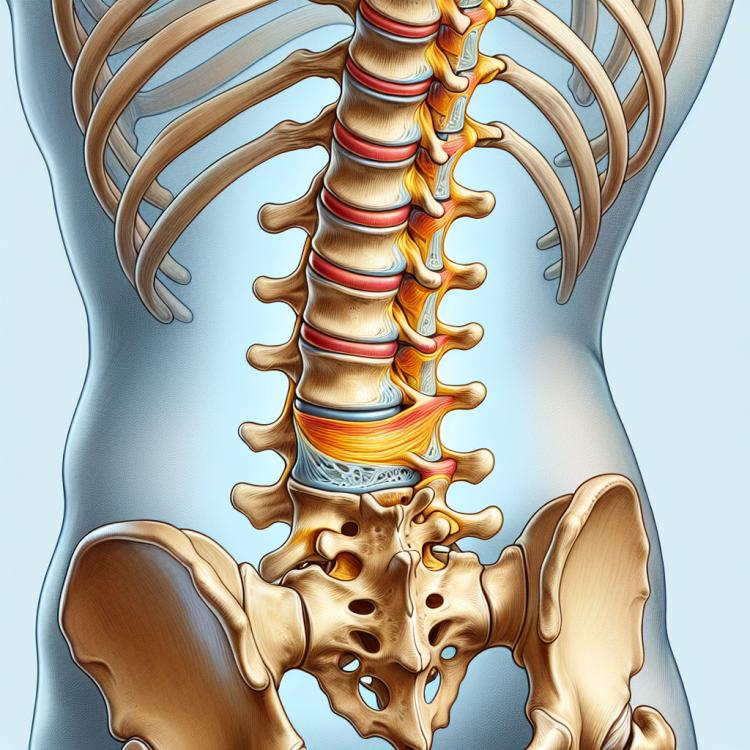
Fundamentals of Understanding Lumbar Spondylosis
Lumbar spondylosis is a degenerative disease of the spine, characterized by changes in the lumbar region of the vertebral column. The main causes of lumbar spondylosis include wear of the intervertebral discs, osteoarthritis, and injuries to the spinal column. Patients with lumbar spondylosis may experience pain in the lumbar area, limited movement, and discomfort during physical activity.
Diagnosis of lumbar spondylosis is based on clinical manifestations, radiological and MRI studies. Treatment of this condition aims at reducing pain, improving spinal mobility, and preventing the progression of degenerative changes. Physical therapy, medication, and in some cases, surgical intervention may be recommended depending on the severity of symptoms and the individual characteristics of the patient.
Factors for the onset of lumbar spondylosis
Lumbar spondylosis, also known as osteochondrosis of the spine, is usually due to degenerative changes in the intervertebral discs and joints. These processes are often associated with natural aging and wear and tear of the cartilage tissue. Additionally, injuries, excessive physical load, posture disorders, and genetic predisposition can contribute to the development of spinal pathology.
- Degenerative changes: Wear of intervertebral discs and joints may be the main cause of lumbar spondylosis.
- Natural aging: With age, the cartilage tissue of the spine loses elasticity and the ability to absorb load.
- Injuries and damage: Injuries to the spine, such as those resulting from an accident or fall, can contribute to the development of spondylosis.
- Excessive physical load: Constant strain on the spine caused by heavy physical work or sports can accelerate degeneration.
- Genetic predisposition: Some people may be more prone to developing lumbar spondylosis due to hereditary factors.
The clinical picture of lumbar spondylosis
The clinical picture of lumbar spondylosis can manifest with various symptoms, including pain in the lumbar region, stiffness of movements, and a feeling of numbness or weakness in the legs. Patients may also experience painful episodes during physical activity or while sitting. Radicular syndrome, caused by spinal nerve compression, can also accompany lumbar spondylosis, which manifests as painful sensations along the nerve and decreased sensitivity in the corresponding area of innervation.
- Low back pain: one of the most common symptoms is pain in the lower back, which can be sharp, dull, or localized.
- Stiffness of movement: patients with lumbar spondylosis may experience limitations in lower back mobility, reducing comfort during everyday movements.
- Feeling of numbness or weakness in the legs: some people with lumbar spondylosis may complain of numbness, tingling, or a feeling of weakness in the legs, especially after physical activity.
- Painful episodes during physical activity: increased pain and discomfort in the lower back during physical activity can also be a symptom of lumbar spondylosis.
- Radicular syndrome: this condition occurs when compression of the spinal nerve leads to pain, numbness, and decreased sensitivity in the corresponding areas of the body, which may be associated with lumbar spondylosis.
The specialists’ perspective on the treatment methods for lumbar spondylosis
Experts in the field of medicine argue that the treatment of lumbar spondylosis should be individualized and include a comprehensive approach aimed at alleviating pain and restoring spinal function. Within the framework of conservative therapy, physiotherapeutic methods, drug therapy, physical activity, and massage are often used with the goal of relieving pain symptoms and enhancing overall muscle tone.
However, in cases of severe disease progression or lack of effect from conservative therapy, specialists may recommend surgical intervention, such as discectomy or spinal stabilization. These methods may be employed to relieve pressure on the spinal cord and nerve roots, improve the quality of life for the patient, and restore spinal function.

Methods for diagnosing lumbar spondylosis
For the diagnosis of lumbar spondylosis, various methods may be used, including clinical examination, X-ray, computed tomography (CT), and magnetic resonance imaging (MRI) of the spine. A clinical examination by a physician can reveal characteristic signs of the disease, such as restricted movement of the spine, pain during movement, and neurological symptoms. X-ray allows for the evaluation of the condition of the bony structures of the spine, while CT and MRI can detect changes in the intervertebral discs, joints, and surrounding tissues.
- Clinical examination: The doctor conducts an examination of the patient for the presence of characteristic symptoms of lumbar spondylosis, such as limited mobility and neurological manifestations.
- X-ray: This method is used to assess the condition of the bony structures of the spine and to identify degenerative changes.
- Computed tomography (CT): Allows for a more detailed image of the spine to identify changes in the intervertebral discs and joints.
- Magnetic resonance imaging (MRI): This method is used for detailed visualization of the soft tissues of the spine, including intervertebral discs and the spinal cord.
- Laboratory tests: Blood tests may sometimes be conducted to rule out other conditions whose symptoms may be similar to lumbar spondylosis.
Methods of treating lumbar spondylosis
- Use of anti-inflammatory drugs: Treatment of lumbar spondylosis may include the use of anti-inflammatory drugs, such as NSAIDs, to reduce pain and inflammation.
- Physical therapy: Physiotherapeutic procedures, such as ultrasound therapy, massage, and therapeutic exercises, can help improve spinal mobility and reduce pain syndrome.
- Corticosteroid injections: Corticosteroid injections in the back area may be prescribed to relieve pain and inflammation in patients with lumbar spondylosis.
- Surgical intervention: In rare cases, when conservative treatment does not lead to improvement, surgical treatment such as discectomy or spinal fusion may be required.
- Training in proper spinal care methods: An important part of treatment is educating the patient in correct methods of back care, including mindful lifting of weights and proper body posture when sitting and standing.
Prevention measures for lumbar spondylosis
- Regular physical exercises: Moderate strengthening exercises for the back and posture correction help maintain spine health.
- Weight control: Maintaining a healthy weight reduces the load on the lumbar spine and decreases the risk of developing lumbar spondylosis.
- Healthy lifestyle: Developing healthy habits, including proper nutrition and quitting bad habits, contributes to overall health strengthening and prevents potential spine issues.
- Workplace ergonomics: Proper furniture layout, use of ergonomic chairs and monitors help avoid improper body positioning and strain on the spine during work.
- Regular medical check-ups: Early detection of the initial signs of disease allows for timely treatment and monitoring of spine condition.