Causes and treatment of perforated gastric ulcer: everything important to know
- The basics of perforated gastric ulcer: definition and causes
- Revealing the causes of perforated gastric ulcer
- Leading signs of perforated gastric ulcer
- Expert opinions on the treatment of perforated gastric ulcer
- Methods for diagnosing perforated gastric ulcer
- The main methods of treating perforated gastric ulcer
- Effective preventive measures for perforated gastric ulcer
- Interesting aspects of gastric perforation.
- FAQ
The basics of perforated gastric ulcer: definition and causes
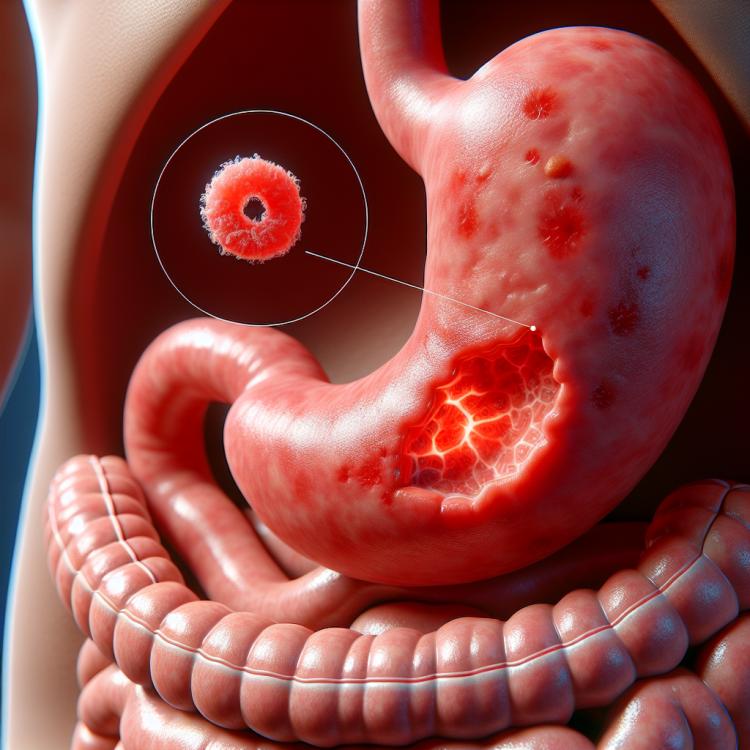
Peptic ulcer of the stomach is an ulcer in which a hole forms in the stomach wall, penetrating through the mucous layer and affecting deeper layers. It manifests as acute pain in the epigastric area, often triggered by food intake or on an empty stomach, which can lead to significant weight loss and gastrointestinal bleeding.
The main causes of gastric perforated ulcer are Helicobacter pylori infection, prolonged use of NSAIDs, stress, and smoking. Disruption of the balance between protective and aggressive factors of the gastric mucosa can lead to the formation of an ulcer defect, requiring comprehensive treatment and monitoring of the patient’s condition.
Revealing the causes of perforated gastric ulcer
A perforated gastric ulcer is an ulcer that penetrates through the mucosal layer of the stomach, usually up to the muscular layer or even into the peritoneal cavity. Its main causes are the bacterium Helicobacter pylori, excessive use of certain medications such as NSAIDs, and prolonged stress. The Helicobacter pylori bacterium contributes to the destruction of the mucosal layer, which promotes the formation of ulcers. The constant use of NSAIDs can also increase the likelihood of developing a perforated ulcer, as these medications can irritate the mucosal layer of the stomach and reduce its protective properties.
Prolonged stress also plays an important role in the development of a perforated ulcer. Increased stress levels can raise acidity levels in the stomach and alter the protective mechanisms of the gastric mucosa, ultimately leading to ulcer formation. It is important to remember that the causes of a perforated gastric ulcer are often interconnected and can reinforce each other, so early consultation with a doctor for diagnosis and treatment is key to preventing complications.
- Helicobacter pylori bacteria: the presence of this bacterium in the stomach can cause inflammation of the mucous membrane and increase the risk of perforating ulcer.
- Use of NSAIDs: prolonged use of non-steroidal anti-inflammatory drugs can damage the gastric mucosa and contribute to the formation of ulcers.
- Prolonged stress: elevated stress levels can increase the acidity of gastric juice and weaken the protective functions of the mucous membrane, which can lead to the formation of ulcers.
- Gastrin: increased secretion of the hormone gastrin can lead to increased acidity in the stomach, which promotes the development of perforating ulcers.
- Smoking and alcohol consumption: smoking and excessive alcohol consumption can have a negative impact on the gastric mucosa, increasing the risk of developing ulcers.
Leading signs of perforated gastric ulcer
Symptoms of perforated gastric ulcers may vary, but typically include burning sensations or pain in the epigastric region, especially after eating. The pain may worsen when fasting or at night. Other characteristic symptoms include nausea, vomiting, a feeling of fullness in the stomach after meals, and changes in weight. It is important to note that perforated ulcers can lead to serious complications, including bleeding or perforation of the stomach wall, which requires immediate medical attention.
Some patients may also experience nonspecific symptoms such as fatigue, anemia, or changes in appetite. Diagnosis of a perforated ulcer includes clinical examination, gastric endoscopy, and, if necessary, other additional tests. If a perforated gastric ulcer is suspected, it is important to see a doctor immediately for timely diagnosis and treatment to prevent possible complications.
- Burning or pain in the epigastric region: often after eating, especially intensifying on an empty stomach or at night.
- Nausea and vomiting: a feeling of nausea, possibly with subsequent vomiting, especially after meals.
- Feeling of fullness in the stomach: a sensation of fullness or bloating in the stomach, even with moderate food intake.
- Weight changes: uncontrolled weight loss or weight gain associated with dietary changes due to ulcer symptoms.
- Fatigue, anemia, and appetite changes: symptoms that may accompany a perforated ulcer, related to impaired digestion and nutrient absorption.
Expert opinions on the treatment of perforated gastric ulcer
Experts in the field of gastroenterology believe that successful treatment of perforated gastric ulcers entails a comprehensive approach, including the eradication of Helicobacter pylori bacteria, reduction of gastric acidity, protection of the gastric mucosa, and prevention of recurrences and complications. One of the main treatment methods for perforated ulcers is the use of antibiotics in combination with proton pump inhibitors to eliminate Helicobacter pylori and reduce acidity. To protect the gastric mucosa, medications that enhance its regeneration and boost its protective properties are usually recommended. Specialists also emphasize the importance of monitoring and preventing recurrences to avoid reformation of the ulcer and potential complications.

Methods for diagnosing perforated gastric ulcer
For the diagnosis of perforated gastric ulcer, methods including clinical examination, gastroscopy, and radiological investigation are widely used. The clinical examination includes taking a medical history, evaluating symptoms, and performing a physical examination, which can assist the doctor in suspecting the presence of a perforated ulcer. Gastroscopy is the gold standard for diagnosing a perforated ulcer, allowing for a visual assessment of the gastric mucosa and the detection of ulcerative defects.
Additional diagnostic methods, such as Helicobacter pylori tests or blood tests for anemia, can aid in specifying the diagnosis. The results of these diagnostic methods, combined with clinical examination, will help the doctor determine the optimal treatment for a patient with a perforated gastric ulcer.
- Clinical examination: Includes gathering medical history, assessing symptoms, and physical examination to identify possible signs of a perforated gastric ulcer.
- Gastrointestinal endoscopy: The gold standard for diagnosing a perforated ulcer, allowing doctors to visually assess the state of the mucosa and detect ulcer defects.
- X-ray examination: A method that allows the visualization of internal organs, including the presence and characteristics of ulcers.
- Tests for Helicobacter pylori: Laboratory tests aimed at detecting the presence of the bacteria often associated with perforated ulcers.
- Blood tests: Including tests for anemia and other parameters that may be altered in the presence of a perforated gastric ulcer.
The main methods of treating perforated gastric ulcer
In addition to pharmacological treatment, an important aspect of treating perforated ulcers is following dietary recommendations, including limiting the intake of spicy, acidic, and fatty foods that can irritate the gastric mucosa. Furthermore, avoiding stressful situations and maintaining a healthy lifestyle also contribute to recovery and the prevention of recurrences of perforated gastric ulcers.
- Use of anti-ulcer medications: includes proton pump inhibitors and antacids to reduce gastric acidity and accelerate ulcer healing.
- Eradication of Helicobacter pylori: is carried out with a combination of medications, including antibiotics and proton pump inhibitors, for the successful elimination of the harmful bacteria.
- Adherence to a diet: involves limiting the intake of spicy, acidic, and fatty foods to avoid irritating the gastric mucosa and to promote recovery.
- Avoiding stressful situations: is important for preventing recurrences of perforated ulcers and maintaining the patient’s overall health.
- Maintaining a healthy lifestyle: includes regular physical activity, avoiding bad habits, and caring for mental and emotional well-being for the successful treatment of gastric perforation ulcers.
Effective preventive measures for perforated gastric ulcer
Other important preventive measures include reducing stress levels, regular physical activity, and the use of medications that help protect the gastric mucosa. Early identification and treatment of Helicobacter pylori infection, which is one of the main causes of perforated ulcers, also plays an important role in the prevention of this disease. Adhering to these recommendations will help reduce the risk of developing a perforated gastric ulcer and maintain gastrointestinal health.
- Avoid smoking and alcohol consumption: Tobacco and alcohol can damage the stomach lining, increasing the risk of developing a perforating ulcer.
- Maintain a healthy diet: Moderate consumption of spicy, fatty, and acidic foods can help prevent irritation of the lining and reduce the likelihood of ulcer formation.
- Manage stress: High levels of stress can increase the likelihood of ulcer formation, so it is important to find ways to reduce stress in daily life.
- Regular physical activity: Exercise contributes to the overall strengthening of the body and can be beneficial in the prevention of gastric perforating ulcers.
- Timely detection and treatment of Helicobacter pylori infection: This infection is often a cause of perforating ulcers, so it is important to get screened in a timely manner and, if necessary, undergo appropriate treatment.
Interesting aspects of gastric perforation.
Another interesting fact is the influence of environmental factors, such as stress, certain infections, and prolonged use of some medications, on the development of a perforated gastric ulcer. The medical community continues to explore the relationship between these factors and the development of the disease in order to develop more effective methods of prevention and treatment of perforated gastric ulcers.