Bedsores: symptoms, causes, and treatment methods
- Understanding pressure ulcers: symptoms, causes, and treatment
- Pathophysiology of pressure ulcers
- Symptoms of pressure sores
- Expert opinions on the treatment of bedsores
- Diagnosis of pressure ulcers
- Treatment of pressure sores
- Prevention of pressure ulcers
- Interesting aspects about pressure ulcers
- FAQ
Understanding pressure ulcers: symptoms, causes, and treatment
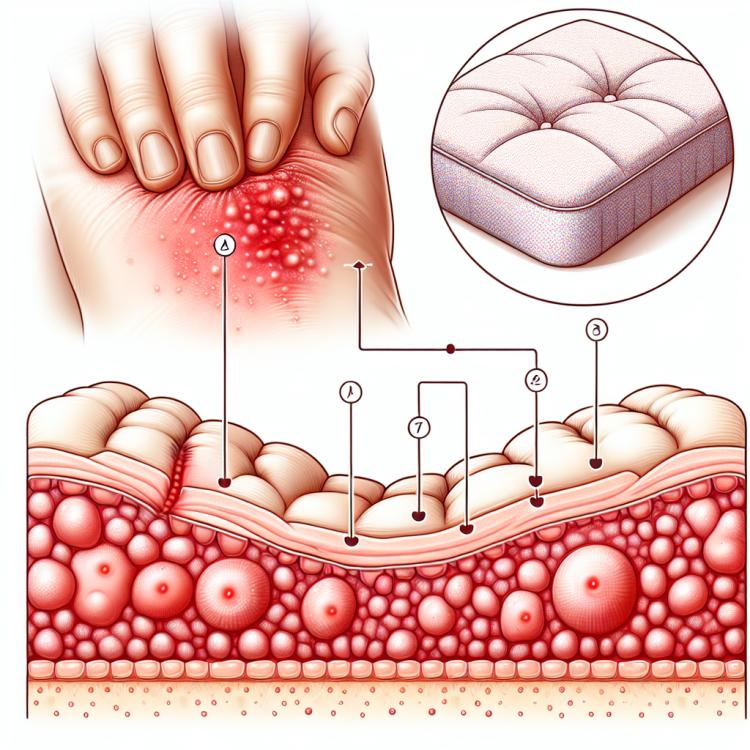
Bedsores, or decubitus ulcers, are complications that often occur in patients with limited mobility, as well as during prolonged bed rest. They typically arise due to constant pressure on certain areas of the skin, leading to hemorrhages, tissue necrosis, and various infections. Manifestations of bedsores can vary, including skin redness, swelling, ulcerative formations, and even purulent processes, which require immediate treatment and preventive measures.
Treatment of bedsores includes various methods, such as regular repositioning of the patient, use of special mattresses and cushions to relieve pressure, as well as meticulous skin care. More severe cases may require surgical intervention. The main principle of treating bedsores is to prevent damage to the skin and tissues, as well as to adopt a timely and comprehensive approach to the problem to minimize complications and accelerate the recovery process.
Pathophysiology of pressure ulcers
Pressure ulcers, or decubitus ulcers, occur as a result of prolonged pressure on the skin and soft tissues, leading to impaired blood supply and tissue oxygenation. The main causes of pressure ulcer development include factors such as patient immobility, the inability to reposition the body, skin moisture, inadequate nutrition and hydration, as well as conditions that make the skin more vulnerable.
Other factors contributing to the occurrence of pressure ulcers include conditions of debilitation, reduced immune system activity, and pathologies that affect the skin’s condition and its resistance to pressure. To prevent pressure ulcers, it is important to conduct regular assessments of at-risk patients, implement preventive measures such as changing body positions, using cushions and special mattresses, as well as proper skin care.
- Pressure on the skin and tissues: prolonged pressure on certain areas of the skin causes ischemia and impaired blood supply.
- Insufficient nutrition and hydration of tissues: lack of nutrients and moisture leads to a decrease in vital processes in cells.
- Reduced immune system activity: weakened immune function lowers the body’s ability to fight infections and tissue damage.
- Skin weakening: age-related changes or pathologies can make the skin more susceptible to pressure and damage.
- Injuries or surgical interventions: tissue damage from injuries or surgeries increases the risk of developing pressure sores.
Symptoms of pressure sores
The symptoms of pressure ulcers depend on the degree and severity of tissue damage. In the early stages of pressure sores, there may be redness of the skin, slight swelling, moderate pain, or a burning sensation in the area of damage. As pressure ulcers progress, the skin may become damaged and ulcerated. Deep pressure ulcers can lead to the formation of an ulcer that penetrates into the deeper layers of tissue and becomes infected.
Patients may also experience reduced sensitivity in the area of the pressure ulcer, which complicates the healing process and increases the risk of complications. It is important to monitor the skin, especially in individuals who are immobile or at risk of developing pressure ulcers, to promptly identify symptoms and prevent the development of complications.
- Skin redness: In the early stages of pressure ulcers, the skin may become red and irritated due to insufficient blood supply.
- Swelling: Swelling of the tissues around the pressure ulcer can be observed, which may indicate a disruption of lymphatic drainage.
- Pain: Patients may experience pain or discomfort in the area of the pressure ulcer, especially when moving or touching the affected area.
- Appearance of an ulcer: In more advanced cases, pressure ulcers can lead to the formation of an ulcer on the skin, which may be weeping and painful.
- Reduced sensitivity: Patients may experience decreased sensitivity in the area of the pressure ulcer due to tissue damage, which increases the risk of complications.
Expert opinions on the treatment of bedsores
Strategies for treating pressure sores, according to experts, should be comprehensive and individualized. Key methods include regular repositioning of the patient, the use of special mattresses and cushions to reduce pressure, and active skin care to prevent the development of ulcers. Experts also recommend conducting medication therapy to control pain and infection, as well as applying methods that stimulate wound healing.
The expert opinion also emphasizes the importance of early detection and treatment of pressure sores to prevent progression and complications. Continuous monitoring of the patient’s condition and regular assessment of treatment effectiveness are key aspects of a successful treatment process. Overall, experts believe that a balanced approach to treating pressure sores, which takes into account medical, preventive, and rehabilitative components, contributes to more effective and favorable outcomes for patients.

Diagnosis of pressure ulcers
Diagnosis of pressure ulcers is typically based on a clinical examination of the skin and tissues in areas suspected of developing pressure ulcers. The doctor may assess the condition of the skin, the presence of redness, ulcerative formations, or purulent discharge. Palpation may also be used to determine the degree of tissue damage and to identify the depth of the pressure ulcers.
Additional diagnostic methods may include the use of instrumental techniques, such as ultrasound examination, to assess damage in the tissues and structures beneath the skin. Diagnosing pressure ulcers is important for choosing the optimal treatment strategy and preventing complications, so early detection and accurate determination of the stage of pressure ulcers are key points in this process.
- Clinical examination: the primary method of diagnosing pressure sores, including a visual assessment of the skin and tissue condition in suspicious areas.
- Palpation: conducting a palpation of the area suspected of having pressure sores to determine the extent of tissue damage.
- Instrumental methods: using ultrasound examination to analyze the contents of damage in the tissues and structures beneath the skin.
- Assessment of damage depth: determining the stage and depth of pressure sores allows for the selection of the best treatment method and forecasting the course of the disease.
- The role of diagnosis: early and accurate identification of pressure sores significantly affects the choice and effectiveness of treatment measures, as well as the prevention of possible complications.
Treatment of pressure sores
In some cases, surgical intervention may be required to remove necrotic tissues or address early-stage deep bedsores. It is important to individualize treatment based on the degree and type of bedsores, as well as to consider the risks of complications and the specific needs of the patient to achieve optimal treatment outcomes.
- Use of special mattresses and pillows: reducing pressure on tissues helps prevent the formation of new bedsores and reduces the risk of damage to vulnerable areas of the skin.
- Regular position changes: turning and repositioning the patient helps reduce pressure on the skin and soft tissues, promoting healing and preventing bedsores.
- Treatment of wounds and ulcers: maintaining cleanliness and antiseptic treatment of damaged skin areas helps prevent infections and promotes tissue healing.
- Optimization of nutrition and hydration: a proper diet with adequate protein, vitamins, and minerals, as well as moderate fluid intake, contribute to tissue regeneration processes and strengthen immunity.
- Surgical intervention: in cases of deep or complicated bedsores, surgical removal of necrotic tissue and special surgical treatment for the wound surface may be required.
Prevention of pressure ulcers
Other important aspects of pressure ulcer prevention include skin care using moisturizing and protective products, regular skin inspections to identify early signs of damage, and maintaining an optimal level of activity and mobility in patients. Prevention of pressure ulcers is a crucial component of care for patients at risk of developing this condition, and timely measures can reduce the likelihood of pressure ulcers occurring and improve the overall condition of patients.
- Regular monitoring of skin condition: it is important to conduct daily skin examinations for patients at risk of pressure sores to detect changes at early stages.
- Changing body position: regularly changing the patient’s position helps reduce pressure on specific areas of the skin and prevent the formation of pressure sores.
- Use of special mattresses and cushions: specialized products help reduce pressure on the skin and tissues, improving blood circulation and preventing damage.
- Proper nutrition and hydration: a balanced diet and adequate fluid intake contribute to skin health and accelerate tissue healing.
- Skin care: regular cleansing and moisturizing of the skin, as well as the use of protective products, help prevent irritation and skin damage.
Interesting aspects about pressure ulcers
Additionally, it is noteworthy that there are several stages of pressure ulcers, ranging from initial signs of redness and skin discoloration to the formation of deep ulcerative defects. Understanding the stages of pressure ulcer development is important for both diagnosis and treatment of this condition, highlighting the significance of careful monitoring and prevention of pressure ulcers in vulnerable patient groups.