Retinal detachment: everything about symptoms, causes, and treatment
- Understanding retinal detachment: causes and consequences
- Factors contributing to retinal detachment
- Main signs of retinal detachment
- Experts’ opinions on the treatment of retinal detachment
- Diagnosis of retinal tear
- Treatment of retinal tear
- Prevention of retinal detachment
- Interesting facts about retinal detachment
- FAQ
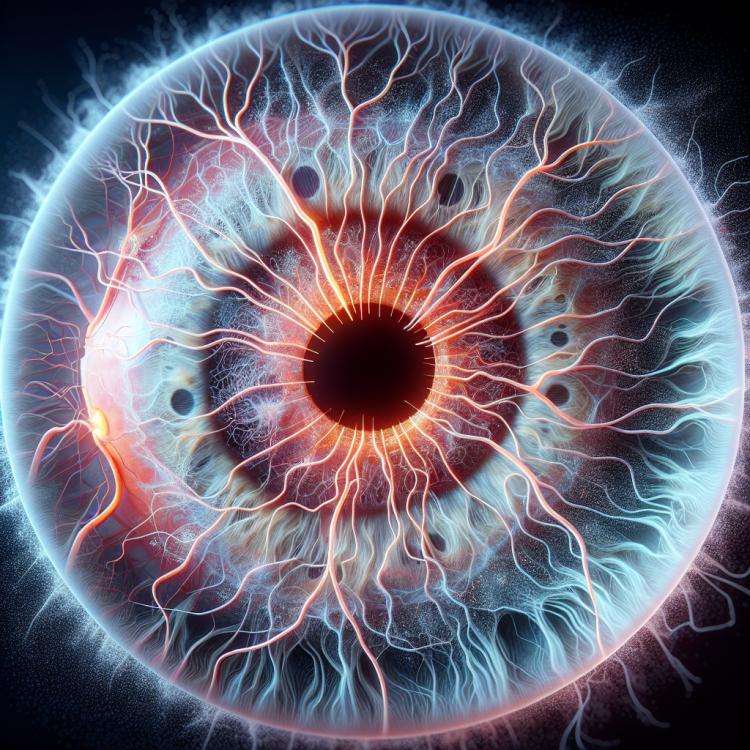
Understanding retinal detachment: causes and consequences
Retinal detachment is a serious condition characterized by the supply of blood to the light-sensitive cells of the eye from the vessels of the choroid. This can occur due to trauma, the growth of a neoplasm, or diabetic retinopathy. With retinal detachment, there is a possibility of developing retinal detachment, which leads to vision loss and requires immediate intervention from a specialist to prevent complications.
Factors contributing to retinal detachment
Retinal detachment can be caused by various factors, including trauma, high intraocular pressure (glaucoma), long anisotropic tension of the retina, age-related changes, and other abnormalities in the structure of the eye. Critical pressure or trauma can lead to the separation of the optical disc boundary and subsequent formation of retinal tears. Additionally, people with high degrees of myopia are at greater risk of retinal detachment due to the anatomical features of the eyeball. It is important to conduct regular preventative examinations with an optometrist or ophthalmologist to detect early warning signs of retinal detachment and receive timely treatment.
- Injuries: physical damage to the eye, such as a blow or wound, can cause a retinal tear.
- High intraocular pressure (glaucoma): increased pressure can lead to a retinal tear due to pressure on the eye tissues.
- Prolonged anisotropic tension of the retina: uneven stretching of the retina can cause it to tear.
- High degree of myopia: individuals with high myopia have an increased risk of retinal tear.
- Abnormalities in the structure of the eye: congenital or acquired abnormalities can contribute to retinal tear due to unusual pressures or tensions in the eye.
Main signs of retinal detachment
Retinal detachment is usually accompanied by a number of characteristic symptoms, which may include tiny lightning-like flashes of light, the appearance of floaters (mosaic glowing shapes) in front of the eyes, as well as a dark shadow that appears in one part of the field of vision. The patient may also experience a sudden drop in vision, as if a part of the visual field has become blurry or closed off. Additionally, the arising changes in visual perception, such as distortion of object sizes or shapes, can also be an indicator of retinal detachment and require immediate consultation with a specialist.
- Tiny lightning-like flashes of light: appear as brief flashes in the field of vision, often associated with retinal detachment.
- Floaters: the appearance of mosaic glowing formations indicates a possible retinal tear and requires attention to the eye’s condition.
- Dark shadow in the field of vision: the appearance of areas of dark shadowing or occlusion of visual perception may be a sign of retinal detachment.
- Sudden decrease in vision: the sensation of loss of clarity in visual subjects may indicate serious vision problems, including retinal detachment.
- Distortion of objects: changes in size or shape of objects during visual perception may signal a possible disruption of the eye’s retina and require consultation with a specialist.
Experts’ opinions on the treatment of retinal detachment
Experts in the field of ophthalmology usually recommend various treatment methods for retinal tears depending on the severity of the case. In the case of small tears without retinal detachment, a laser coagulation procedure is performed, aimed at strengthening the retina and preventing further tears. In the case of retinal detachment, experts typically recommend surgical intervention, such as vitrectomy, to restore the position of the retina and prevent vision loss. However, the precise treatment is usually prescribed individually, after a comprehensive clinical examination of each case.

Diagnosis of retinal tear
Diagnosis of retinal detachment requires a comprehensive approach and specialized research methods. Determining a retinal tear may include conducting an examination of the eye’s fundus using specialized equipment, such as a binocular loupe or a biomicroscope. Additional methods, such as optical coherence tomography (OCT) or retinal angiography, may be used for more accurate identification of tears and assessment of the state of the eye’s vessels, which allows for determining the treatment strategy and preventing potential complications.
- Fundus examination: conducted using specialized equipment to visualize tears or defects in the retina.
- Optical coherence tomography (OCT): allows obtaining detailed images of the eye structures, including the retina and its condition, which helps detect tears and assess their nature.
- Retinal angiography: a method used to assess the condition of the blood vessels in the fundus, which helps identify circulatory disorders and possible factors contributing to retinal tears.
- Vision testing: an important part of the diagnostics, allowing for the assessment of the patient’s level of vision and changes caused by retinal tears.
- Intraocular pressure measurement: in some cases, measuring intraocular pressure may be conducted to assess the state of the eye and identify associated risks.
Treatment of retinal tear
- Surgical intervention: Depending on the size and nature of the tear, various surgical procedures are performed, including laser coagulation, cryotherapy, or surgical repositioning of the retina.
- Injections into the eye: Sometimes injections are used to stabilize the retina and prevent the development of new tears.
- Rest and activity restrictions: After surgery, patients may be recommended to limit physical activity and visual stress to prevent recurrences and facilitate healing.
- Regular monitoring and control: After treatment, it is important to follow the specialist’s recommendations and undergo regular examinations to monitor the condition of the retina and identify potential complications.
- Adherence to rehabilitation recommendations: Patients may be offered a rehabilitation program aimed at supporting visual functions and overall eye health after treatment.
Prevention of retinal detachment
- Regular ophthalmological examinations: Conducting scheduled examinations with an ophthalmologist will help identify predisposition to retinal detachment and take measures to prevent its occurrence.
- Healthy lifestyle: Proper nutrition rich in antioxidants, avoidance of harmful habits such as smoking, and moderate physical exercises contribute to strengthening eye tissue and reducing the risk of retinal detachment.
- Avoiding eye injuries and overload: Preventing eye injuries and avoiding excessive strain on the visual system will help prevent retinal detachment.
- Monitoring high intraocular pressure: Patients with glaucoma or elevated intraocular pressure should regularly monitor their condition and follow their doctor’s recommendations to prevent possible complications, including retinal detachment.
- Timely consultation with a specialist: If any changes occur in vision or any unpleasant symptoms related to the eyes emerge, it is necessary to consult an ophthalmologist for professional advice and diagnosis.
Interesting facts about retinal detachment
An interesting fact is that retinal detachment can manifest with minor symptoms, such as tiny lightning-like flashes of light or the appearance of floaters in the vision, which can be the first warning sign of a possible tear. This highlights the importance of careful monitoring of eye health and seeking immediate attention from an ophthalmologist in case of such symptoms.