Rheumatic carditis: diagnosis, treatment, and prevention
- Rheumatic carditis: main aspects and definition
- Etiology of rheumatic carditis
- The clinical picture of rheumatic carditis
- Expert recommendations for the treatment of rheumatic heart disease
- Methods for diagnosing rheumatic carditis
- Approaches to the treatment of rheumatic carditis
- Measures for the prevention of rheumatic carditis
- 5 fascinating facts about rheumatic heart disease
- FAQ
Rheumatic carditis: main aspects and definition
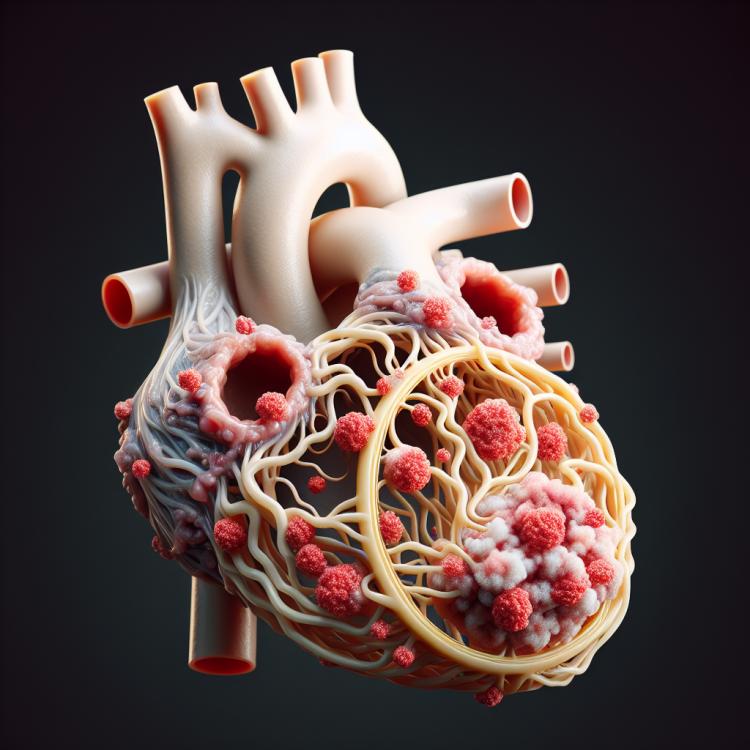
Rheumatic carditis is an inflammatory disease of the heart muscle, valves, or membranes, most often caused by a bacterial infection. The pathogenesis of rheumatic carditis is associated with the immune response of the body to the antigens of microorganisms that penetrate the heart tissues. In rheumatic carditis, inflammation and destruction of heart tissue cells occur, which can lead to serious complications such as valve damage, thrombosis, and arrhythmias.
Etiology of rheumatic carditis
Rheumatic carditis is an inflammatory disease of the heart that usually develops as a complication after a streptococcal infection, such as streptococcal pharyngitis or rheumatic fever. The pathogenesis of rheumatic carditis is associated with the immune response, where antibodies produced against the infection are directed against heart tissue, resulting in inflammation of the myocardium, valves, or pericardium.
Other possible causes of rheumatic carditis may include infections caused by bacteria, viruses, fungi, or parasites. In some cases, rheumatic carditis may develop as an autoimmune disease, when the immune system attacks its own heart tissues. Genetic predisposition may also play a role in the development of rheumatic carditis.
- Streptococcal infection: Rheumatic heart disease is often associated with a preceding streptococcal infection, such as streptococcal pharyngitis.
- Immune response: The pathogenesis of rheumatic heart disease is related to the immune response, where antibodies attack heart tissue, causing an inflammatory reaction.
- Infections of various natures: Rheumatic heart disease can be a result of infections caused by bacteria, viruses, fungi, or parasites.
- Autoimmune disorders: In rare cases, rheumatic heart disease may develop as an autoimmune condition, where the immune system attacks its own heart cells.
- Genetic predisposition: Some individuals may have a genetic predisposition to develop rheumatic heart disease.
The clinical picture of rheumatic carditis
The clinical picture of rheumatic carditis can manifest with various symptoms, including fatigue, shortness of breath, chest pain, possible arrhythmias, and the appearance of edema. The main clinical manifestations of rheumatic carditis are signs of damage to different parts of the heart, such as the myocardium, endocardium, and pericardium.
Patients with rheumatic carditis may also experience significant weakness, increased fatigue even with minimal physical activity, reduced appetite, and weight loss. It is important to note that the symptoms of rheumatic carditis can vary depending on the individual characteristics of the patient and the extent of damage to the heart tissue.
- Shortness of breath: a feeling of lack of air or difficulty breathing, especially during physical activity
- Chest pain: uncomfortable sensations, pressure, or discomfort in the chest that may worsen with physical exertion
- Arrhythmia: disturbances in heart rhythm, such as rapid heartbeat, irregular pulsations, or interruptions in heart activity
- Swelling: swelling of tissues due to fluid retention, most commonly observed in the area of the legs, calves, or ankles
- Fatigue: increased weakness, tiredness, and reduced physical endurance, even with minimal exertion
Expert recommendations for the treatment of rheumatic heart disease
The opinion of experts on the treatment of rheumatocarditis is based on a comprehensive approach that includes antibacterial therapy to eliminate the pathogen, antiplasmotropic drugs to reduce inflammation, and glucocorticoids to control the immune response. It is important to individualize treatment methods depending on the severity of the disease, the presence of complications, and the patient’s characteristics.
Experts also emphasize the importance of regular monitoring of patients after the completion of rheumatocarditis treatment to detect recurrences and prevent possible complications. Continuous medical supervision and adherence to all specialists’ recommendations will help improve the prognosis of the disease and minimize the risk of recurrent cases of rheumatocarditis.

Methods for diagnosing rheumatic carditis
A comprehensive approach is used for the diagnosis of rheumatic heart disease, which includes clinical manifestations, laboratory, and instrumental examination methods. The basis of diagnosis is the medical history, physical examination, and assessment of symptoms such as shortness of breath, fatigue, pain, or swelling, as well as heart auscultation to identify changes in its sounds.
Laboratory methods include determining the levels of inflammatory markers, such as C-reactive protein and erythrocyte sedimentation rate, as well as serological tests for the presence of antibodies to possible infectious agents. Instrumental diagnostics may include ECG, echocardiography to assess the condition of the heart and valves, as well as magnetic resonance or computed tomography for additional imaging.
- Medical history and clinical examination: an important component of diagnosis, includes analysis of the patient’s complaints, the history of the disease, and physical examination of the heart.
- Laboratory studies: include the determination of inflammatory markers such as C-reactive protein and erythrocyte sedimentation rate, as well as serological tests for antibodies to infectious agents.
- Electrocardiography (ECG): allows evaluation of the electrical activity of the heart and identification of possible rhythm and conduction abnormalities.
- echocardiography (EchoCG): the method of choice for visualizing the structures of the heart, allows assessment of heart size, valve function, and detection of changes characteristic of rheumatic carditis.
- Magnetic resonance imaging (MRI) and computed tomography (CT): can be used for additional visualization of the heart and assessment of structural changes when rheumatic carditis is suspected.
Approaches to the treatment of rheumatic carditis
Medication therapy often includes antibiotics to combat infection, anti-inflammatory drugs to reduce inflammation, medications to improve heart function and control rhythm, as well as drugs to relieve swelling. It is essential to ensure the patient gets adequate rest, adheres to the recommended supportive therapy regimen, and follows the doctor’s recommendations to achieve the best outcomes in the treatment of rheumatic carditis.
- Medication therapy: includes the use of antibiotics to combat infectious agents and anti-inflammatory drugs to reduce inflammation in the heart.
- Cardiac drugs: to improve heart function and control heart rhythm, treatment with medications such as beta-blockers or antiarrhythmic drugs may be prescribed.
- Diuretics: help reduce swelling and eliminate excess fluid in the body, which can be important in rheumatic heart disease.
- Provision of rest: it is important to ensure the patient has a rest regimen to promote recovery and improve heart function.
- Surgical intervention: in some cases, surgical treatment may be required, for instance, to repair or replace a damaged heart valve.
Measures for the prevention of rheumatic carditis
To prevent rheumatic heart disease, it is also important to follow hygiene rules, including regular hand washing, avoiding close contact with infected individuals, and adhering to general precautions to prevent infections. Special attention should also be paid to the prevention of rheumatic fever, as early detection and treatment of this condition help reduce the risk of developing rheumatic heart disease.
- Timely treatment of infections: It is important to treat infections, especially those of streptococcal nature, promptly to prevent the possible development of rheumatic fever and, consequently, rheumatic heart disease.
- Regular diagnosis and treatment of throat and dental diseases: Effective treatment of infections in the throat and oral cavity can help prevent possible heart damage, including rheumatic heart disease.
- Hygiene practices: Regular handwashing, avoiding close contact with infected individuals, and following basic precautions can help prevent infections that may lead to the development of rheumatic heart disease.
- Prevention of rheumatic fever: Early detection and treatment of rheumatic fever play a crucial role in preventing the development of subsequent complications, including rheumatic heart disease.
- Avoiding risk factors: Avoiding factors that may increase the likelihood of infections and inflammations will help reduce the risk of developing rheumatic heart disease.
5 fascinating facts about rheumatic heart disease
Interestingly, rheumatic carditis primarily affects children and young adults, especially those who have a predisposition to autoimmune diseases such as rheumatoid arthritis. Besides infectious causes, rheumatic carditis can also be triggered by autoimmune reactions when the immune system attacks its own heart tissues. Such facts highlight the importance of early diagnosis and adequate treatment of rheumatic carditis to prevent serious consequences for the heart.