Scar on the uterus: causes, symptoms, and treatment methods
- Understanding Uterine Scars: Key Aspects
- Etiology of uterine scar
- Clinical picture of a scar on the uterus
- Approaches of specialists to the treatment of scar on the uterus
- Methods for diagnosing a scar on the uterus
- Methods of treating a uterine scar
- Measures for prevention of uterine scarring
- Unusual aspects of a uterine scar.
- FAQ
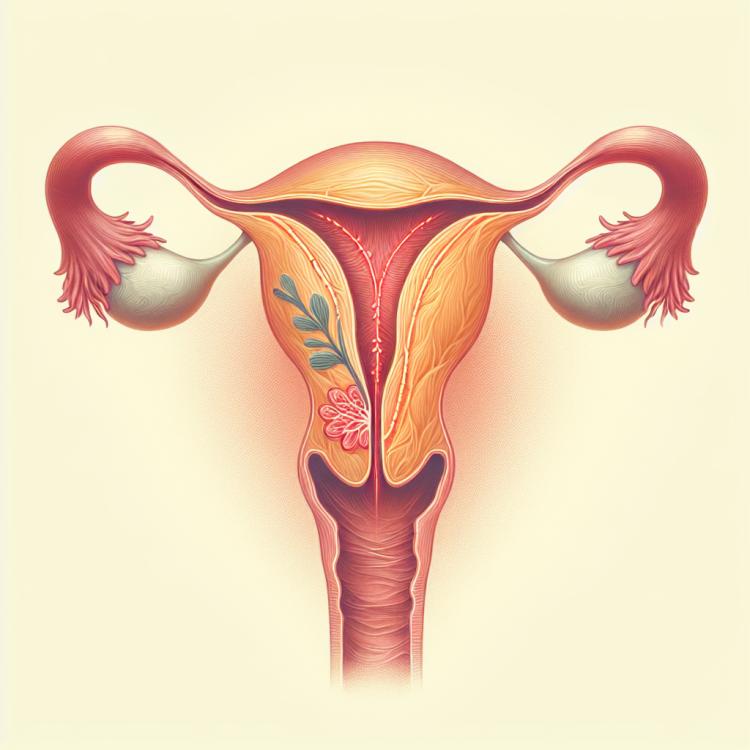
Understanding Uterine Scars: Key Aspects
A scar on the uterus is a formation of tissue that usually occurs as a result of the childbirth process or surgical intervention, such as a cesarean section. Scars on the uterus can be a source of various problems, such as painful menstruation, infertility, and an increased risk of complications during pregnancy and childbirth.
Understanding the main aspects of a scar on the uterus is essential for effectively managing its consequences. It is important to consider the patient’s clinical history, symptoms, possible complications, and diagnostic methods to determine the optimal treatment approach for this condition.
Etiology of uterine scar
A scar on the uterus, or uterine scar, is a formation of connective tissue that occurs as a result of healing after injuries or surgeries on the uterus. The main causes of the formation of a scar on the uterus are cesarean section, abortions, polyp removal, congenital anomalies of the uterus, inflammatory processes, and other interventions in the structure of the uterus. Disruption of the healing process after such interventions leads to the formation of scar tissue, which can further affect a woman’s health and her reproductive function.
- Surgical interventions: Include cesarean section, uterine surgeries, removal of polyps, which can lead to the formation of scar tissue on the uterus.
- Abortions: Termination of pregnancy, especially abortions that are accompanied by complications or incomplete miscarriages, can be a cause of scarring.
- Inflammatory processes: Inflammation of the uterus, endometritis, or other infectious diseases can lead to the formation of scar tissue on the uterus.
- Congenital anomalies: Some congenital defects of the uterus or reproductive system may be a primary cause of scarring.
- Excessive stretching of the uterus: Enlargement of the uterus, for example, during a multiple pregnancy, can affect the healing process after childbirth and lead to the formation of scar tissue.
Clinical picture of a scar on the uterus
In women with a uterine scar, a variety of clinical manifestations may be observed depending on the size, location, and degree of impact of the scar. In most cases, the uterine scar does not present any obvious symptoms and is discovered incidentally during a gynecological examination or ultrasound. However, in some cases, women may experience painful menstruation, lower abdominal pain, heavy or irregular bleeding, improper fetal position during pregnancy, or recurrent miscarriages. It is important to note that the symptoms of a uterine scar can be diverse and require a competent diagnostic approach for accurate determination and management of this condition.
- Painful menstruation: some women with a scar on the uterus may experience increased pain and dysmenorrhea during menstruation.
- Heavy or irregular bleeding: a scar on the uterus may be associated with anomalies in the menstrual cycle, manifesting as excessive or irregular bleeding.
- Lower abdominal pain: women with a scar on the uterus may experience discomfort or pain in the lower abdomen, especially during menstruation or sexual intercourse.
- Abnormal fetal position: a scar on the uterus may affect pregnancy development, leading to abnormal fetal positioning or complications during childbirth.
- Recurrent miscarriages: some studies show a connection between a scar on the uterus and recurrent miscarriages due to its impact on the structure and functionality of the uterus.
Approaches of specialists to the treatment of scar on the uterus
The approaches to treating a uterine scar depend on the clinical manifestations, size and location of the scar, as well as the reproductive plans of the patient. An expert approach to treating a uterine scar may include conservative treatment using hormonal medications, laser therapy, or physiotherapy. In cases where the scar causes significant symptoms or complicates pregnancy, surgical intervention may be required, such as hysteroscopy or myomectomy.
Treatment of a uterine scar is a complex process that requires an individual approach and risk assessment. Experts believe that effective management of a uterine scar can improve a woman’s health, reduce the risk of complications, and help achieve a desired pregnancy. Therefore, it is important that treatment is conducted under strict medical supervision and guidance from experienced specialists, taking into account the individual characteristics of each patient.

Methods for diagnosing a scar on the uterus
Various methods are used to diagnose a scar on the uterus, including gynecological examination, ultrasound (transvaginal or transabdominal), magnetic resonance imaging (MRI), and computed tomography (CT). A gynecological examination allows the doctor to assess the anatomical structure of the uterus and detect possible changes, including a scar on the uterus. Ultrasound is widely used to determine the size, shape, and structure of the scar, as well as its impact on reproductive function and the pelvic organs. MRI and CT provide detailed information about the structure of the uterus and the scar, which helps the doctor determine the optimal treatment plan for each specific situation.
- Gynecological examination: This method allows the doctor to conduct an initial assessment of the structure of the uterus and detect the presence of scars.
- Ultrasound examination: Vaginal or transabdominal ultrasound is used for a more accurate determination of the size, shape, and structure of the scar on the uterus.
- Magnetic resonance imaging (MRI): MRI provides a more detailed image of the structure of the uterus and the scar, which helps in determining the optimal treatment.
- Computed tomography (CT): CT also provides detailed information about the scar on the uterus, which aids in diagnosis and treatment selection.
- Hysteroscopy: This method allows direct visual examination of the uterine cavity and identification of changes, including the presence of scars.
Methods of treating a uterine scar
- Conservative methods: Include the use of medications to improve tissue condition and reduce inflammation.
- Surgical intervention: May be required in the presence of significant scar size or its impact on a woman’s reproductive function.
- Scar resection: One of the surgical treatment methods, where part of the uterine scar is removed.
- Hysteroscopy: Used to remove scar tissue from the uterine cavity through minimally invasive intervention.
- Uterine resection: In some cases, the removal of part or the entire uterus may be required due to a scar that poses a serious threat to a woman’s health.
Measures for prevention of uterine scarring
Another important aspect of preventing uterine scarring is the timely treatment of inflammatory processes in the pelvic organs and the uterus. Preventing infections and timely treatment of diseases that may lead to the formation of scar tissue can reduce the risk of this condition and its negative consequences for a woman’s health.
- Avoid unnecessary surgical interventions: minimizing the number of procedures, such as cesarean sections, reduces the risk of scarring on the uterus.
- Follow postoperative care recommendations: strict adherence to the doctor’s instructions after surgical interventions helps prevent complications and scarring on the uterus.
- Regular check-ups and consultations: timely examinations and diagnostics allow for the identification of changes in the uterus and the initiation of treatment before scarring occurs.
- Prevention of inflammatory processes: preventing infections and treating pelvic diseases reduces the likelihood of scarring on the uterus.
- Maintaining overall health: a healthy lifestyle, proper nutrition, regular physical activity, and avoidance of harmful habits contribute to overall health and reduce the risk of various complications, including scarring on the uterus.
Unusual aspects of a uterine scar.
Moreover, a scar on the uterus can cause various symptoms, including painful menstruation, bleeding, and lower abdominal pain. Interestingly, some women may not experience any symptoms even in the presence of a scar on the uterus, highlighting the importance of regular check-ups and preventive measures to identify and manage this condition.