Chronic Pelvic Pain Syndrome: Understanding, Diagnosis, and Treatment
- Analysis of chronic pelvic pain syndrome
- Etiology of Chronic Pelvic Pain Syndrome
- Concepts of the symptoms of chronic pelvic pain syndrome
- On the treatment of chronic pelvic pain syndrome: expert opinions
- Methods for diagnosing chronic pelvic pain syndrome
- Effective methods for treating chronic pelvic pain syndrome
- Measures to prevent chronic pelvic pain syndrome
- Unusual aspects of chronic pelvic pain syndrome
- FAQ
Analysis of chronic pelvic pain syndrome
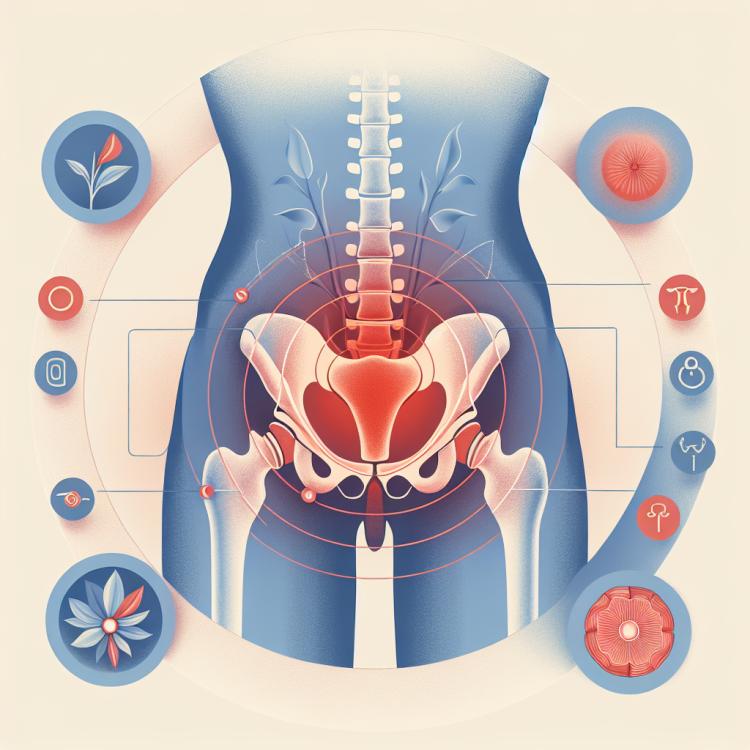
The chronic pelvic pain syndrome (CPPS) is a common condition characterized by painful sensations in the pelvic area that can persist for six months or more. CPPS is a complex syndrome, often triggered by a combination of physiological, psychological, and social factors. This syndrome can significantly impact the quality of life of patients and may require a comprehensive and multifaceted approach to diagnosis and treatment.
Understanding the pathogenesis and mechanisms of CPPS remains a subject of study for the medical community. Diagnosing this syndrome requires careful analysis of symptoms, exploration of the medical history, and conducting appropriate examinations. Treatment of CPPS is usually multifactorial, including pharmacotherapy, physiotherapy, psychological support, and rehabilitation. An individualized approach to each patient and understanding the underlying mechanisms of this syndrome are key components of successful management and treatment of this condition.
Etiology of Chronic Pelvic Pain Syndrome
The syndrome of chronic pelvic pain is a multifaceted condition, and its etiology can be multifactorial. The main causes include inflammatory processes, pelvic muscle dysfunction, nerve compression, psychosocial factors, and even disorders in the functioning of the pelvic organs. Conditions such as chronic inflammation, tissue damage, nervous system pathologies, and psychosocial stresses may be among the possible causes of this syndrome.
For the accurate identification of the causes of chronic pelvic pain syndrome, a comprehensive diagnosis is important, including medical examination, laboratory and instrumental methods, as well as consultation with specialists of various profiles. Identifying the primary pathological process underlying the syndrome allows for the development of an effective treatment plan aimed at reducing pain and improving the patient’s quality of life.
- Inflammatory processes: Chronic inflammation of the pelvic organs can lead to the development of pain syndrome.
- Pelvic muscle dysfunction: Tension and spasms of the pelvic floor muscles can cause chronic pelvic pain.
- Nerve compression: Compression of nerve structures in the pelvic area can be one of the causes of pain.
- Psychosocial factors: Stress, depression, anxiety can contribute to the development of chronic pelvic pain syndrome.
- Internal organ disorders: Pathologies of the pelvic organs, such as endometriosis, cysts, adenomyosis, can be a cause of chronic pelvic pain.
Concepts of the symptoms of chronic pelvic pain syndrome
Symptoms of chronic pelvic pain syndrome can vary and be individual for each patient. Most often, patients complain of pain in the pelvic region, difficulty urinating, painful sexual intercourse, as well as changes in bowel function. The presence of pain, which can be sharp, dull, stabbing, or aching, is often associated with chronic pelvic pain syndrome.
Additional symptoms may include bladder dysfunction, pain during defecation, neurological manifestations, such as nerve irritation or discomfort in the pelvic area. It is important to pay attention to the nature and intensity of symptoms, as this will help the doctor to more accurately diagnose and develop an effective treatment plan for each patient.
- Pain in the pelvic area: patients may experience various types of pain, such as sharp, dull, stabbing, or pulling pain.
- Difficulties with urination: there may be problems with urination, including frequent, painful, or incomplete emptying of the bladder.
- Painful sexual intercourse: patients may experience pain or discomfort during sexual intercourse, which may be associated with chronic pelvic pain syndrome.
- Changes in bowel function: symptoms may include pain during defecation, constipation, or diarrhea, which may result from pelvic organ dysfunction.
- Bladder dysfunction: feelings of frequent urination, nighttime urination (nocturia), strong urges to urinate, or urinary incontinence may be signs of the syndrome.
On the treatment of chronic pelvic pain syndrome: expert opinions
The treatment of chronic pelvic pain syndrome represents a complex task that requires an individual approach for each patient. Expert opinions in the field of medicine emphasize the importance of a comprehensive approach that includes medication, physiotherapy, psychotherapy, as well as specialized methods like trigger point therapy or neuromodulation. An important aspect is also educating patients on self-pain management and stress control.
Experts agree that effective treatment of chronic pelvic pain syndrome may vary depending on the pathogenesis, underlying cause of the disease, and the psycho-emotional state of the patient. An individual approach to each case, considering all accompanying factors, a commitment to improving patients’ quality of life, and lasting remission are the main principles that experts in the treatment of chronic pelvic pain syndrome build their opinions upon.

Methods for diagnosing chronic pelvic pain syndrome
The diagnosis of chronic pelvic pain syndrome is a multifaceted process that includes a comprehensive examination of the patient taking into account various aspects, including medical history, physical examination, and the conduct of specialized tests. The main diagnostic methods include a digital examination of the pelvic area, laboratory tests to check for possible inflammatory processes, as well as instrumental methods such as ultrasound and magnetic resonance imaging for additional assessment of the condition of the tissues and organs in the pelvic region.
An important aspect of diagnosing chronic pelvic pain syndrome is also taking into account various factors, including psychosocial aspects and the patient’s life circumstances. The approach to diagnosis should be comprehensive, allowing for the identification of the underlying cause of pain and determining an individualized treatment approach for each patient.
- Medical history and physical examination: An important stage of diagnosis is the detailed discussion of symptoms with the patient and the physical examination to identify characteristic signs.
- Laboratory tests: Blood and urine tests can help identify possible inflammatory processes or infections that may be related to chronic pelvic pain syndrome.
- Ultrasound examination: An ultrasound can be used to assess the condition of the pelvic organs and investigate accompanying pathologies.
- Magnetic resonance imaging (MRI): MRI provides detailed images of the structures in the pelvic area and can be useful in finding possible causes of pain.
- Consultation with specialists: Consulting a urologist, gynecologist, neurologist, and other specialists may be necessary to determine a diagnosis and develop a treatment plan.
Effective methods for treating chronic pelvic pain syndrome
An important aspect of treating chronic pelvic pain syndrome is a patient-centered approach that includes understanding the individual needs and preferences of the patient. Educating patients on pain self-management strategies, support, and motivation play a significant role in the long-term success of treatment. Collaboration among an interdisciplinary team of specialists allows for the development of an optimal treatment plan aimed at minimizing pain symptoms and enhancing the quality of life for patients with chronic pelvic pain syndrome.
- Pharmacological treatment: The use of medications to relieve pain, such as analgesics, anti-inflammatory agents, muscle relaxants.
- Physical therapy: The application of various physical methods, such as exercises to strengthen pelvic muscles, massage, as well as electrotherapy and ultrasound therapy.
- Psychotherapy: Psychological support and therapy can help patients cope with pain syndrome, reduce stress and anxiety levels.
- Injection procedures: Nerve blocks, botulinum toxin injections, or probiotics may be used to reduce pain and improve the function of pelvic organs.
- Surgical intervention: In some cases, surgical treatment may be necessary, such as nerve decompression or correction of anomalies causing pain syndrome.
Measures to prevent chronic pelvic pain syndrome
It is also important to avoid prolonged sitting or standing in one position, to adhere to proper ergonomics when working at a computer or performing daily tasks to avoid overloading the pelvic area. Consulting with physical therapy specialists to develop individualized exercises and recommendations for preventing pelvic pain can also help prevent the onset of this syndrome and maintain the health of the pelvic area.
- Active lifestyle: regular physical exercises contribute to strengthening the pelvic muscles and maintaining overall body tone.
- Maintaining normal weight: excess weight can create additional stress on the pelvic area, increasing the risk of pain development.
- Preventing chronic inflammatory diseases: timely treatment of infections and inflammatory processes will help prevent complications, including chronic pelvic pain syndrome.
- Consulting a doctor at the first symptoms: timely examination will allow identifying and resolving the issue before it progresses.
- Maintaining proper ergonomics: adhering to the correct posture while performing everyday tasks will help prevent unnecessary strain in the pelvic area.
Unusual aspects of chronic pelvic pain syndrome
Another unusual aspect of chronic pelvic pain syndrome is its multifaceted nature, where pain sensations can vary from severe to mild, from sharp to dull, and from transient to constant. This variety of symptoms requires careful medical examination and a differentiated approach to treatment for each patient with chronic pelvic pain syndrome.