Understanding postnasal drip syndrome: causes, symptoms, and modern treatment methods
- Clarification of the concept of postnasal syndrome
- Etiology of postnasal syndrome
- Clinical picture of post-nasal syndrome
- Expert recommendations for treating post-nasal syndrome
- Methods for diagnosing postnasal syndrome
- Options for treating post-nasal syndrome
- Preventive measures for postnasal syndrome
- Amazing aspects of postnasal syndrome
- FAQ
Clarification of the concept of postnasal syndrome
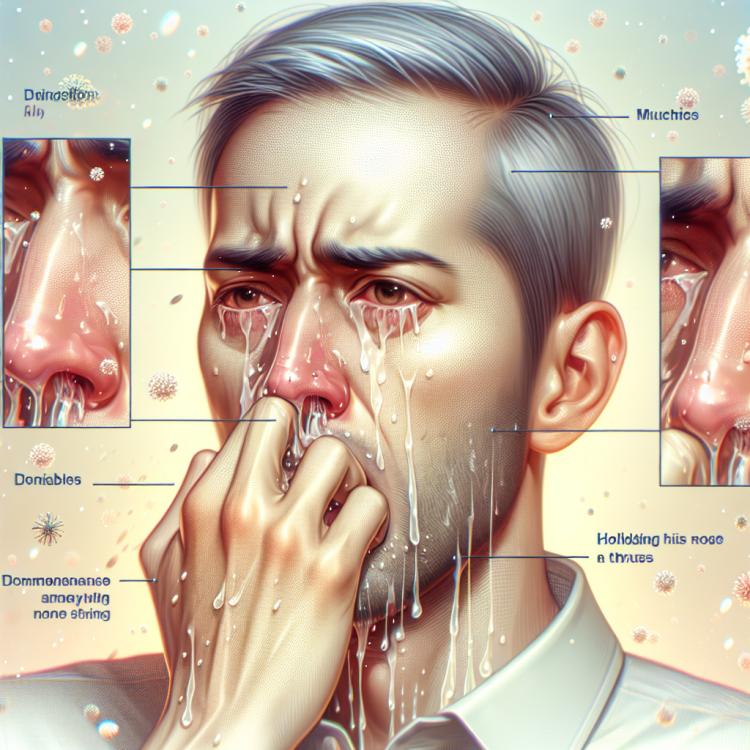
Postnasal syndrome (PNS) is a condition characterized by excessive mucus dripping from the back of the nasal cavity down the back of the throat. This syndrome is often accompanied by various symptoms such as a constant feeling of mucus in the throat, cough, respiratory difficulties, and changes in voice. In addition to infectious causes, PNS can be triggered by allergic reactions, acid reflux from the stomach, and other factors, making its diagnosis and treatment multifaceted and requiring a personalized approach.
Etiology of postnasal syndrome
The causes of post-nasal syndrome can be varied and may include various diseases of the respiratory tract, allergic reactions, disturbances in the mechanisms of the nasal mucosa, as well as side effects of certain medications. Disorders of mucociliary clearance, upper respiratory infections, inhalation of irritants, and tobacco smoke can also contribute to the development and exacerbation of post-nasal syndrome symptoms.
- Allergic reactions: allergens such as dust, pollen, St. John’s wort, or mold can cause inflammation and exacerbate post-nasal syndrome.
- Respiratory diseases: chronic rhinitis, sinusitis, adenoids, as well as other diseases of the nose and throat can contribute to the onset of post-nasal syndrome symptoms.
- Medication effects: the use of certain medications, such as blood thinners or blood pressure medications, can cause dryness of the mucous membrane, exacerbating the symptoms of post-nasal syndrome.
- Mucociliary clearance disorders: difficulty in clearing the nose and throat of mucus and microorganisms can lead to the accumulation of secretions and worsen the symptoms of post-nasal syndrome.
- Tobacco smoke: exposure to tobacco smoke on the nasal mucosa can provoke irritation and worsen the condition in post-nasal syndrome.
Clinical picture of post-nasal syndrome
Symptoms of post-nasal syndrome may include a constant feeling of nasal congestion, a sense of mucus accumulation in the throat, sneezing, coughing, occasional laryngeal cough, worsening of smell, a feeling of irritation and dryness in the throat. Patients may also experience discomfort when breathing through the nose, feelings of weakness or fatigue, and a non-productive cough. It is noted that symptoms may be exacerbated in certain conditions, such as lying down and contact with irritants in the environment.
- Nasal congestion: a constant feeling of difficulty breathing through the nose.
- Accumulation of mucus: the sensation of mucus in the throat, causing discomfort and inconvenience.
- Sneezing and coughing: reflex actions that play an important role in clearing the upper respiratory tract of irritants.
- Deterioration of smell: changes in the perception of odors due to disruptions in the breathing processes in the nasal passages.
- Non-productive cough: characterized by the absence of mucus expectoration, often accompanying post-nasal syndrome.
Expert recommendations for treating post-nasal syndrome
Expert opinions on the treatment of post-nasal syndrome emphasize the importance of a comprehensive approach, which may include the use of anti-inflammatory agents, mucolytics, antihistamines, airway clearance medications, and, in some cases, glucocorticoids. Experts also pay attention to an individualized approach to treatment, considering the characteristics of each specific case and the benefits of various therapeutic methods in the context of the patient’s overall clinical status.
Additionally, experts stress the need for regular monitoring of treatment efficacy and adjustments to the therapy plan as needed. The patient’s lifestyle, including allergic reactions to the environment and habits, is also an important aspect that specialists take into account when developing an individualized treatment plan for post-nasal syndrome.

Methods for diagnosing postnasal syndrome
Diagnosis of post-nasal syndrome typically includes an examination and patient history, as well as an assessment of symptoms such as nasal congestion, mucus accumulation in the throat, cough, and other associated manifestations. To clarify the diagnosis, radiological and endoscopic examinations of the nasopharynx, sinus computed tomography, allergy tests, and other methods that allow the exclusion of other diseases with similar symptoms may be conducted.
Additionally, laboratory tests can be useful for identifying possible allergic reactions or infectious processes that may exacerbate the symptoms of post-nasal drip syndrome. In some cases, a consultation with an otolaryngologist or allergist may be necessary for a more detailed examination and clarification of the treatment approach for this condition.
- Patient history and examination: Conducting a detailed examination and collecting the patient’s history to identify characteristic symptoms and preceding factors.
- X-ray examination of the nasopharynx: A method of survey radiography that can be used to assess the condition of the nasopharynx and indications for further procedures.
- Endoscopic examination of the nasopharynx: Visualization of the nasopharynx using an endoscope, allowing for a detailed investigation of the condition of the nasal passages and throat.
- Computed tomography of the sinuses: A method for obtaining detailed images of the nasal cavity sinuses, which helps identify possible changes and pathologies.
- Laboratory tests: Include a complete blood count, biochemical indicator tests, allergy tests, analysis of nasal mucus for the presence of infection pathogens, and other laboratory research methods.
Options for treating post-nasal syndrome
- Pharmacotherapy: Includes the use of antihistamines to reduce allergic reactions, inhalations of glucocorticosteroids to decrease inflammation, decongestants to relieve nasal congestion, and antiseptics to combat microbial flora.
- Physiotherapy: Involves rinsing the nasal passages with saline solutions for cleansing, inhalations with added essential oils to reduce inflammation, and breathing exercises to enhance oxygen flow and improve gas exchange.
- Avoiding irritants: Avoiding tobacco smoke, polluted air, and other environmental irritants may help reduce the symptoms of postnasal syndrome.
- Surgical intervention: In cases where conservative treatment does not yield the desired effect, surgical treatment such as correction of intranasal defects, polypectomy, or other procedures may be required.
- Consultation with specialists: Patients with postnasal syndrome may benefit from consulting with an otolaryngologist, allergist, or pulmonologist to determine the optimal treatment strategy and manage symptoms.
Preventive measures for postnasal syndrome
It is important to strive to maintain a healthy breathing environment by avoiding exposure to irritants, dust, and tobacco smoke. Regular visits to a doctor to monitor the condition of the respiratory organs and timely seeking medical help at the first signs of possible problems can help prevent the development of post-nasal syndrome.
- Maintaining a healthy lifestyle: Regular physical exercise, a balanced diet, and avoiding harmful habits such as smoking and alcohol consumption contribute to the overall strengthening of the body and reduce the risk of developing post-nasal syndrome.
- Avoiding contact with allergens: Preventing exposure to allergens such as dust, plant pollen, microbes, and mold can reduce the risk of allergic reactions, which may lead to post-nasal syndrome.
- Maintaining nasal hygiene: Regularly cleaning the nasal cavity from dust and mucus, using products to moisturize the mucous membrane can help reduce irritation and congestion.
- Maintaining a healthy breathing environment: Avoiding smoke, vapors of irritating substances, regular ventilation of rooms, and humidifying the air contribute to reducing potential irritants, lowering the risk of post-nasal syndrome symptoms.
- Regular check-ups and consultations with a doctor: Timely seeking medical help at the first signs of respiratory issues and regular preventive visits to a specialist help identify potential health problems at early stages and take measures to address them.
Amazing aspects of postnasal syndrome
Another surprising aspect of post-nasal syndrome is its impact on the quality of life of patients. Constant feelings of discomfort, nasal congestion, coughing, and other symptoms can significantly impair a person’s comfort and well-being, affecting their psycho-emotional state and social aspects of life, making timely and effective treatment of post-nasal syndrome especially important.