Irritable Bowel Syndrome: Causes, Symptoms, and Treatment Methods
- Understanding the essence of irritable bowel syndrome
- Pathophysiology of Irritable Bowel Syndrome
- The main symptoms of irritable bowel syndrome.
- Optimal methods for treating irritable bowel syndrome
- Methods for diagnosing irritable bowel syndrome
- Methods of treating irritable bowel syndrome
- Measures to prevent irritable bowel syndrome
- Amazing facts about irritable bowel syndrome
- FAQ
Understanding the essence of irritable bowel syndrome
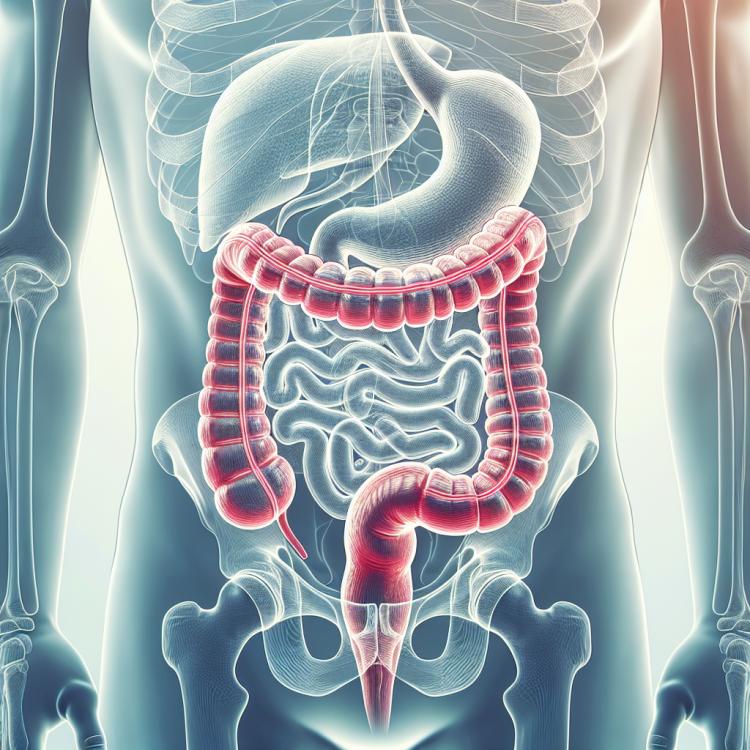
Irritable bowel syndrome (IBS) is a functional disorder of the digestive system, characterized by chronic discomfort in the abdominal area, accompanied by changes in the rhythm of defecation. This syndrome can manifest with a variety of symptoms, such as pain or discomfort in the abdomen, bloating, and unstable stool. Although the exact causes of IBS are not fully established, it is believed that various factors influence its development, including disturbances in the nervous regulation of the digestive tract, psycho-emotional factors, and changes in the gut microbiome.
Pathophysiology of Irritable Bowel Syndrome
Irritable bowel syndrome (IBS) is a chronic functional disorder of the intestine characterized by abdominal pain and changes in intestinal functions without organic causes. The pathophysiology of IBS includes hypersensitivity of the intestine, changes in intestinal motility, disturbances in the interaction between the brain and the intestine, inflammation of the intestinal mucosa, dysbiosis, and psychosomatic factors. Possible factors, including food intolerance, stress, changes in the composition of the intestinal microbiome, genetic factors, and certain infections, can exacerbate symptoms and trigger disease flare-ups, making it multifactorial and rather complex to treat.
- Intestinal hypersensitivity: Patients with irritable bowel syndrome may have increased sensitivity of the sacral bowel, leading to an enhanced pain response upon stimulation.
- Changes in intestinal motility: Patients with IBS may experience disruptions in peristalsis and coordination of bowel movements, causing symptoms of diarrhea, constipation, or both.
- Disruptions in the brain-gut interaction: Dysfunction of specific regulatory mechanisms, such as the “brain-gut” interaction, may lead to exacerbation of IBS symptoms.
- Inflammation of the intestinal mucosa: Possible inflammation of the intestinal mucosa affects digestive functions and may contribute to the onset of the disease.
- Dysbiosis: Disruptions in the composition and balance of microorganisms in the gut can influence IBS symptoms due to improper digestion and assimilation of food.
The main symptoms of irritable bowel syndrome.
The main symptoms of irritable bowel syndrome include pain and discomfort in the abdominal area. Patients may experience rumbling, bloating, constipation, diarrhea, or alternating episodes of these symptoms. Symptoms may worsen after eating or during stressful situations. Additionally, patients with IBS often face a feeling of incomplete bowel evacuation, which can lead to dissatisfaction after defecation.
The painful symptoms of IBS can significantly impact the quality of life of patients, often leading to psychological issues and social isolation. Understanding these symptoms and their timely diagnosis is essential for establishing the correct differential diagnosis and selecting the optimal treatment strategy.
- Pain and discomfort in the abdominal area: Patients often experience various types of pain – colicky, cramping, or stretching sensations in the abdominal area.
- Gurgling and bloating: The feeling of gurgling and bloating in the abdomen are typical symptoms of IBS.
- Constipation: Difficulties with the frequency and texture of stools may occur in patients with irritable bowel syndrome.
- Diarrhea: Episodes of frequent and watery stools are also seen in IBS patients.
- Feeling of incomplete evacuation: Patients may experience a sensation that the intestines are not fully cleared after a bowel movement.
Optimal methods for treating irritable bowel syndrome
Experts in the field of gastroenterology recommend a comprehensive approach to treating irritable bowel syndrome, taking into account the individual characteristics of each patient. Optimal treatment methods may include dietary changes, pharmacological medications, psychological support, and lifestyle modifications. For most patients, adjusting the diet and excluding certain foods can significantly alleviate symptoms.
An important aspect of treating irritable bowel syndrome is maintaining regular communication with a gastroenterology specialist to adjust therapy according to the dynamics of the condition. Some patients may benefit from psychotherapeutic support for managing stress and anxiety, which also contributes to improving quality of life and reducing symptoms of irritable bowel syndrome.

Methods for diagnosing irritable bowel syndrome
The diagnosis of irritable bowel syndrome involves a comprehensive approach, including history-taking, physical examination, laboratory, and instrumental studies. Often, various methods are used to exclude organic diseases, such as blood tests, stool tests for hidden blood, colonoscopy, and gastrointestinal tract examination using various imaging techniques.
To assess bowel function and identify pathological changes, studies such as rectosigmoidoscopy, capsule endoscopy, computed tomography, and others may be conducted. An important step in the diagnosis is the mandatory exclusion of other possible causes of symptoms, such as inflammatory bowel diseases, tumors, infections, etc. All these methods assist doctors in accurately diagnosing irritable bowel syndrome and developing an individualized treatment strategy for each patient.
- Anamnesis and physical examination: The doctor evaluates the main symptoms and medical history, conducts an abdominal examination and other clinical checks.
- Laboratory studies: Blood tests (e.g., complete blood count and inflammatory marker analysis), stool test for hidden blood to rule out organic causes of symptoms.
- Colonoscopy: Endoscopic examination of the large intestine and its upper parts, which allows the doctor to assess the condition of the mucosa, take biopsy samples, and identify any changes.
- Rectosigmoidoscopy: Endoscopic examination of the rectum and colon area using a flexible fiber colonoscope to diagnose changes and inflammation.
- Computed tomography: A method of studying internal organs using X-rays to identify changes in the intestines and surrounding tissues.
Methods of treating irritable bowel syndrome
Effective management of irritable bowel syndrome requires an individualized approach that takes into account the characteristics of each patient and their symptoms. A combination of different treatment methods, including lifestyle changes, medications, and therapies for stress reduction, may be necessary. It is important that decisions about treatment methods are made in collaboration with a doctor, considering all circumstances of the condition and the specifics of each case.
- Diet: Implementing dietary changes, including a low FODMAP diet or the elimination of certain foods, may help improve symptoms.
- Probiotics: Taking probiotics helps restore healthy gut microflora and may reduce symptoms of IBS.
- Pharmacological treatment: The use of antidepressants and antispasmodics helps reduce pain sensations and improve the frequency and consistency of stools.
- Stress therapy: Psychotherapeutic methods such as cognitive behavioral therapy or relaxation techniques can help manage stress that may exacerbate symptoms.
- Individual approach: Treatment of irritable bowel syndrome requires a personalized approach that takes into account the individual characteristics of each patient and their response to various treatment methods.
Measures to prevent irritable bowel syndrome
It is also advisable to consult a doctor at the first symptoms of IBS for timely diagnosis and development of an individualized treatment strategy. Regular medical supervision will allow monitoring the condition and effectively managing the disease, minimizing its negative impact on the patient’s daily life.
- Healthy eating: Adhering to a balanced diet that includes enough vegetables, fruits, fiber, excluding food allergens and potentially harmful products.
- Stress management: Applying relaxation techniques, meditation, yoga, and stress management therapy to reduce the negative impact of stressful situations on the gastrointestinal tract.
- Physical activity: Regular moderate physical exercise helps normalize intestinal peristalsis and improves overall health.
- Avoiding certain foods: Taking into account individual food tolerances, excluding or limiting the consumption of products that may exacerbate IBS symptoms, such as caffeine, alcohol, carbonated drinks, and fatty foods.
- Regular consultations: Patients predisposed to IBS or already diagnosed should consult a doctor for recommendations on prevention and management of gastrointestinal conditions.
Amazing facts about irritable bowel syndrome
Furthermore, an interesting factor influencing IBS is its connection with psychological factors such as stress and anxiety. Studies show that there is a correlation between the patient’s emotional state and the severity of IBS symptoms, highlighting the importance of psycho-emotional status in managing this condition.