Synovitis: causes, symptoms, and treatment methods
- Understanding Synovitis: Key Concepts
- Conditions for the occurrence of synovitis
- Signs and symptoms of synovitis
- Recommendations from specialists for the treatment of synovitis
- Methods of diagnosing synovitis
- Methods of treating synovitis
- Methods of preventing synovitis
- Amazing aspects of synovitis
- FAQ
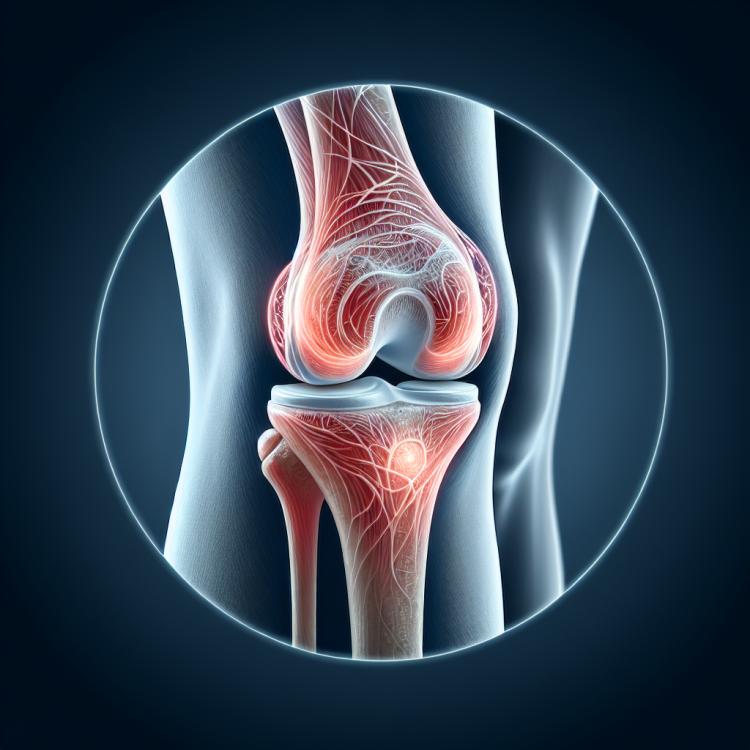
Understanding Synovitis: Key Concepts
Synovitis is an inflammatory disease of the joint capsule, accompanied by swelling, pain, and limited movement in the joint. This condition can be caused by various factors, including injuries, infections, or autoimmune processes. Understanding the fundamental concepts of synovitis is essential for determining effective treatment methods and preventing complications, such as joint deformity and chronic pain, caused by prolonged inflammation.
Conditions for the occurrence of synovitis
Synovitis is an inflammatory disorder of the joint synovial membrane, caused by various reasons. One of the most common causes of synovitis is trauma or traumatic injury to the joint, which can lead to inflammation of the synovial membrane as a reaction to tissue damage. Other causes include rheumatic diseases, infections, and certain metabolic disorders that can cause inflammation in the joints and accompanying synovitis. Depending on the etiology, the causes of synovitis can vary, and accurately identifying them is important for the appropriate selection of treatment and prognosis of the disease.
- Injuries and joint damage: Physical damage to joints can trigger an inflammatory reaction of the synovial membrane.
- Rheumatic diseases: Autoimmune rheumatic diseases, such as rheumatoid arthritis, can provoke synovitis.
- Infections: Bacterial, viral, or fungal infections can cause inflammation of the joints and synovitis.
- Metabolic disorders: Some metabolic disorders, such as gout, can lead to the formation of crystals in the joints and cause synovitis.
- Repetitive joint movements: Excessive use or monotonous movements of the joints can also be a cause of inflammation and synovitis.
Signs and symptoms of synovitis
The symptoms of synovitis can manifest in various ways, including pain in the affected joint, swelling, a feeling of warmth around the joint, limitations in movement, as well as creaking or clicking when moving. Patients may experience symptoms depending on the severity and duration of the inflammatory process in the joint. Pain typically intensifies with movement or load on the joint, and morning stiffness of the joint may also be observed, which gradually decreases with movement.
Additionally, in synovitis, general symptoms may be observed, such as an increase in body temperature, general weakness, aches, and fatigue, indicating a systemic response to the inflammatory process. It is important to pay attention to the symptoms characteristic of synovitis and, if possible, consult a doctor to establish an accurate diagnosis and develop an optimal treatment plan.
- Joint pain: synovitis is often accompanied by painful sensations in the affected joint that intensify with movement or load.
- Swelling and edema: joint synovitis is often accompanied by swelling of the tissues around the joint, which can lead to an increase in the size of the joint and a feeling of tension in it.
- Sensation of warmth in the joint: the affected joint may feel warm to the touch due to the active inflammatory process in the synovial membrane.
- Limitation of movement: synovitis can lead to restricted mobility of the joint due to pain, swelling, and inflammation, which makes normal joint functioning difficult.
- Crepitus or clicks during movement: some patients may notice crackling or popping sounds when moving the affected joint, which is related to changes in the structure of the joint tissues.
Recommendations from specialists for the treatment of synovitis
Expert opinions on the treatment of synovitis are based on a comprehensive approach to managing the inflammatory process in the joints. The main treatment strategies include the use of anti-inflammatory medications to reduce inflammation and pain, physiotherapy procedures to strengthen and restore joint functions, as well as possible surgical intervention in case conservative treatment is ineffective. Experts recommend an individualized approach to synovitis treatment, taking into account the disease characteristics of each patient and aiming at improving quality of life and preserving joint mobility.
The importance of timely consultation with a doctor for the diagnosis of synovitis and determination of the optimal treatment plan is emphasized. Experts advise not to delay a visit to a specialist at the first signs of joint inflammation to prevent the progression of the disease and reduce the risk of complications. Timely and adequate treatment of synovitis according to specialists’ recommendations can help improve the prognosis of the disease and lessen its negative impact on the patient.

Methods of diagnosing synovitis
The diagnosis of synovitis includes a set of activities, starting with a clinical examination and patient history. Important diagnostic methods are a general blood and urine test, which can reveal signs of inflammation in the body, such as an increased number of leukocytes and C-reactive protein. In addition, additional instrumental methods, such as X-ray, magnetic resonance imaging (MRI), or arthroscopy, can help visualize inflammatory changes in the joint and further confirm the diagnosis of synovitis.
One of the important aspects of diagnosing synovitis is the differential diagnosis with other diseases, such as arthritis or traumatic joint injuries. Accurately determining the causes of symptoms and carefully studying clinical and laboratory data will assist specialists in making the correct diagnosis and selecting the optimal treatment for the patient.
- Clinical examination: The doctor conducts a physical examination of the joint to identify signs of inflammation, assess range of motion limitations, and detect pain upon palpation.
- Laboratory studies: A complete blood and urine analysis helps determine the level of inflammation in the body, including an increased number of leukocytes and infectious markers.
- Instrumental methods: X-ray of the joints can help identify degenerative changes, while MRI or arthroscopy allow for visualization of inflammatory changes in the synovial membrane.
- Joint biopsy: In rare cases, taking a tissue sample for laboratory analysis may be required to clarify the diagnosis and exclude other pathologies.
- Differential diagnosis: Conducting a comparative analysis with other diseases, such as arthritis, helps exclude other causes of symptoms and establish an accurate diagnosis of synovitis.
Methods of treating synovitis
- Use of NSAID medications: Nonsteroidal anti-inflammatory drugs, such as ibuprofen and diclofenac, can help reduce inflammation and alleviate joint pain in synovitis.
- Use of corticosteroid injections: In cases of rheumatoid synovitis, corticosteroid injections may be used to reduce inflammation and improve joint function.
- Physical therapy and rehabilitation: Physiotherapeutic procedures, exercises, and massage can help restore the function of the affected joint and strengthen the surrounding tissues.
- Surgical intervention: In some cases, especially with significant joint damage, surgical treatment such as arthroscopy or synovial tissue removal may be necessary.
- Treatment of the underlying condition: In synovitis associated with rheumatic or metabolic disorders, it is important to treat the underlying condition for effective relief of synovitis symptoms.
Methods of preventing synovitis
Regular check-ups and consultations with a doctor will help timely identify any early signs of inflammation or joint degeneration and take the necessary measures. Adhering to proper techniques when performing exercises, using protective equipment during sports activities, as well as avoiding prolonged standing or sitting in improper positions can reduce the likelihood of developing synovitis and support joint health in the long term.
- Physical activity: Regular moderate physical exercises help strengthen muscles and ligaments, preventing stress on the joints.
- Proper nutrition: A balanced diet rich in vitamins and minerals supports joint health and overall well-being.
- Avoiding injuries: Maintaining caution and using protective gear during sports or other activities can help prevent joint damage.
- Maintaining a healthy lifestyle: Weight control, quitting bad habits, and regular medical check-ups can help maintain joint health.
- Adhering to proper technique in physical exercises: Proper positioning and execution of exercises help avoid overstrain and joint injuries, reducing the risk of developing synovitis.
Amazing aspects of synovitis
Another fascinating aspect of synovitis is its connection with various rheumatic diseases, which emphasizes the importance of differential diagnosis and an individualized approach to treatment. Understanding the mechanisms of synovitis development and its impact on the joints not only allows for effective treatment of this condition but also opens up prospects for the development of new methods for the prevention and treatment of joint diseases.