Sclerosis of the bladder neck: features and treatment methods
- Basics of bladder neck sclerosis
- Factors causing bladder neck sclerosis
- The main signs of bladder neck sclerosis
- Expert opinion on treatment methods for bladder neck sclerosis
- Methods for diagnosing bladder neck sclerosis
- Methods of treating bladder neck sclerosis
- Methods for preventing bladder neck sclerosis
- Unknown aspects of bladder neck sclerosis
- FAQ
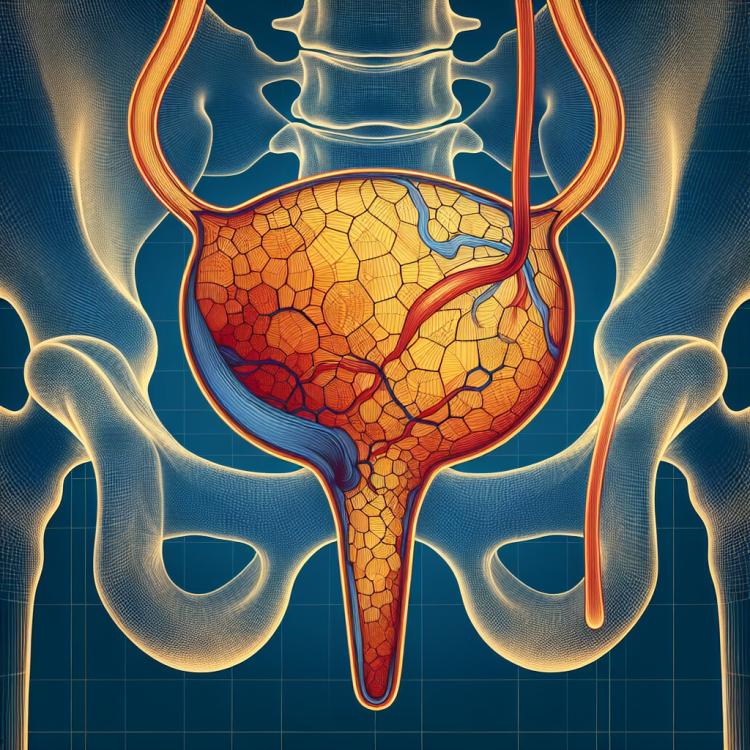
Basics of bladder neck sclerosis
Sclerosis of the bladder neck is a condition characterized by the formation of dense tissues around the bladder neck, leading to its narrowing. This can cause an obstruction to normal urine flow and lead to various symptoms, including pain during urination and urethral incompetence.
The causes of bladder neck sclerosis can be varied, including inflammation, trauma, surgical interventions, or even uncontrolled cell growth behavior. Treatment for bladder neck sclerosis may include conservative methods, such as physiotherapy and medication, as well as surgical interventions to remove obstructions and restore normal organ function.
Factors causing bladder neck sclerosis
Sclerosis of the bladder neck is a pathological condition caused by various factors. The main factors contributing to the development of this disease are neurodegenerative processes, inflammatory reactions, and autoimmune disorders. For example, multiple sclerosis can lead to damage to nerve fibers, including those that control bladder function, which contributes to the development of sclerosis of the bladder neck. In addition, infections, injuries, and genetic factors can also play a role in the formation of this condition.
- Neurodegenerative processes: the destruction of nerve cells can hinder the normal transmission of signals between the brain and the bladder, contributing to the development of bladder neck sclerosis.
- Inflammatory reactions: chronic inflammation in the body can lead to damage to the bladder tissues and surrounding organs, accelerating the development of structural changes.
- Autoimmune disorders: malfunction of the immune system can lead to its attack on the body’s own tissues, including the walls of the bladder.
- Infections: the presence of recurrent urinary tract infections can promote the development of inflammatory processes and subsequent sclerosis of the bladder neck.
- Traumas: injuries to the bladder caused by trauma can lead to its degeneration and the development of pathological changes, including sclerosis of the bladder neck.
The main signs of bladder neck sclerosis
Symptoms of bladder neck sclerosis may include urethral disturbances, a feeling of incomplete bladder emptying after urination, urinary incontinence, as well as pain or discomfort in the bladder area. Uncontrolled urination, frequent urination, and uncontrollable urination during coughing or sneezing may also be among the manifestations of bladder neck sclerosis. Differential diagnosis of these symptoms requires a comprehensive approach taking into account the patient’s medical history, physical examination, and additional methods of investigation such as ultrasound, cystoscopy, and urodynamic tests.
- Dysuric disorders: include difficulties with urination, changes in the frequency of urination, and painful urination.
- Sensory disturbances: discomfort, pain, or unusual sensations during urination may occur.
- Urinary incontinence: the possibility of accidental urinary incontinence due to incomplete emptying of the bladder.
- Feeling of incomplete bladder emptying: patients may experience a sensation that the bladder is not completely emptied after urination.
- Uncontrolled urination: the possibility of accidental and unpredictable urination during efforts such as coughing or sneezing.
Expert opinion on treatment methods for bladder neck sclerosis
Experts in the field of urology and neurology emphasize that the treatment of sclerosis of the bladder neck requires a comprehensive approach that takes into account both symptomatic therapy and the primary impact on the cause of the disease. In modern medicine, pharmacological drugs, physiotherapeutic methods, surgical correction, and psychological support for the patient may be used to treat this condition.
The expert opinion highlights the importance of an individual approach to each patient when choosing treatment methods for sclerosis of the bladder neck. Based on clinical data, the degree of pathology development, and concomitant diseases, doctors can recommend an optimal treatment course aimed at improving the quality of life for patients, including controlling symptoms and preventing complications.

Methods for diagnosing bladder neck sclerosis
Diagnosis of bladder neck sclerosis includes various methods, starting from the patient’s history and physical examination, and ending with instrumental studies such as ultrasound diagnostics, cystoscopy, and urodynamic tests. These methods allow for determining the extent of damage to the bladder neck, identifying the presence of possible complications, and planning an effective treatment strategy for each specific case of bladder neck sclerosis. Differentiating this condition from other pathologies of the urinary system is also an important stage of diagnosis and requires a comprehensive approach and professional analysis of all available data.
- Medical history and physical examination: The doctor collects medical history and conducts a physical examination, identifying characteristic symptoms of bladder neck sclerosis.
- Ultrasound diagnostics: This method allows for the visualization of the bladder structure and assessment of its functioning, which aids in the diagnosis of bladder neck sclerosis.
- Cystoscopy: An endoscopic examination that allows for direct visualization of the bladder neck condition and identification of changes characteristic of this disease.
- Urodynamic tests: Tests to assess the function of the bladder and adjacent organs of the urinary system, which help detect urodynamic disturbances related to bladder neck sclerosis.
- Laboratory tests: The use of various laboratory studies to identify inflammatory processes, infections, or other pathologies that may be associated with bladder neck sclerosis.
Methods of treating bladder neck sclerosis
- Medication therapy: Includes the use of medications to improve control over urination and reduce bladder dysfunction.
- Urodynamic training: Training aimed at improving muscle control of the bladder and reducing urinary incontinence.
- Physiotherapy: The use of physical treatment methods to improve bladder function and reduce symptoms of bladder neck sclerosis.
- Botulinum toxin injection: This method may be used to paralyze the bladder muscles and improve control over urination.
- Surgical intervention: In some cases, surgical intervention is required to restore bladder function, for example, by correcting anomalies or resecting affected tissues.
Methods for preventing bladder neck sclerosis
- Maintaining a healthy lifestyle: regular physical activity, healthy eating, and giving up bad habits can help maintain bladder function and strengthen the urinary tract.
- Regular medical check-ups: timely visits to the doctor for regular check-ups and examinations can help detect the early signs of bladder neck sclerosis and take measures to prevent them.
- Avoiding hypothermia: maintaining normal body temperature and avoiding hypothermia helps strengthen the immune system and reduce the risk of inflammatory processes in the urinary tract.
- Cautious approach to stress levels: managing stress and psycho-emotional state can have a positive effect on bladder function and prevent its dysfunction.
- Adhering to urinary tract hygiene: regularly following hygiene rules to prevent urinary tract infections helps reduce the likelihood of conditions that threaten bladder health.