Fistula of the rectum: features, symptoms, and treatment methods
- Explanation of the concept “Anal fistula
- Factors contributing to the development of rectal fistula
- The main signs of a rectal fistula
- The specialists’ view on the methods of treating anal fistula
- Methods for diagnosing rectal fistula
- Main methods of treating rectal fistula
- Methods for preventing rectal fistula
- Amazing aspects of rectal fistula
- FAQ
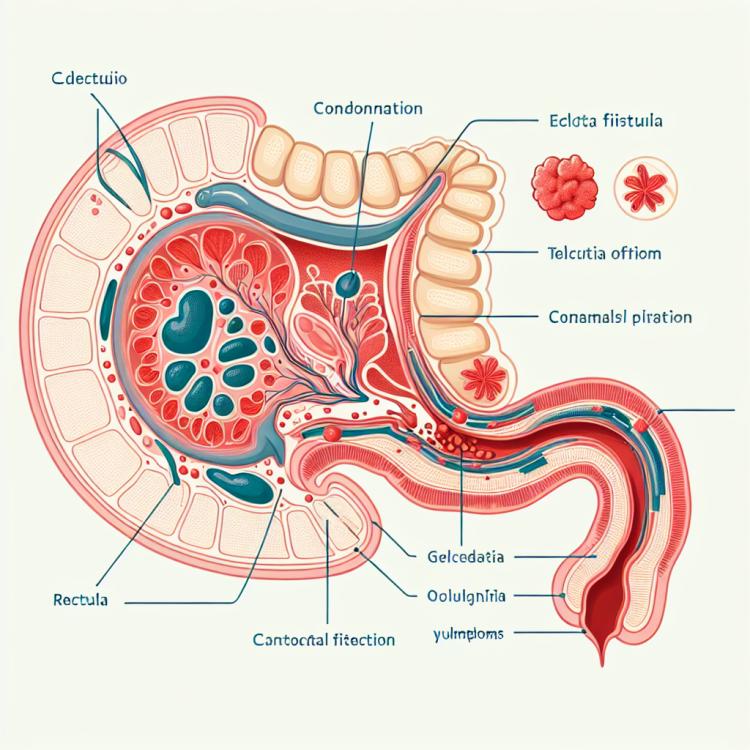
Explanation of the concept “Anal fistula
A rectal fistula is a type of surgical disease characterized by the pathological creation of a passage between the rectum and adjacent organs, such as the bladder or vagina. This pathological passage, usually caused by an inflammatory process, is a channel through which the contents of the rectum can leak into other cavities, causing discomfort and a range of characteristic symptoms for this condition. Treatment of a rectal fistula depends on the severity of the case, but may include conservative methods such as the use of medications, or in some cases, surgical intervention aimed at restoring the normal anatomy of the rectum and adjacent organs.
Factors contributing to the development of rectal fistula
Factors contributing to the development of rectal fistula include inflammatory bowel diseases such as ulcerative colitis and Crohn’s disease. These conditions can cause the formation of ulcerative defects in the rectum, which may then lead to the formation of a fistula. Trauma in the rectal area, surgical interventions in this region, or infectious processes can also contribute to the occurrence of a rectal fistula. It is important to note that personal hygiene and prevention of bowel diseases are significant in preventing the possible development of this pathological condition.
- Inflammatory bowel diseases: The occurrence of a rectal fistula is often associated with ulcerative colitis or Crohn’s disease, which lead to ulcer formation and subsequent fistula formation.
- Injuries in the area of the rectum: Surgical interventions, injuries, or other damage in this area may contribute to fistula formation.
- Infectious processes: Some infections in the rectal area can lead to inflammation and the development of a fistula.
- Inadequate treatment of bowel diseases: If inflammatory or infectious bowel diseases do not receive proper treatment, this can cause complications, including fistula formation.
- Genetic predisposition: Some genetic factors may increase the risk of developing a rectal fistula in certain individuals.
The main signs of a rectal fistula
The main symptoms of a rectal fistula may include the discharge of purulent-mucous masses from the rectum, bleeding, pain in the anal area, sometimes accompanied by itching and discomfort. These symptoms may be periodic or appear after a bowel movement. Discharges with an unpleasant odor may also be one of the signs of a rectal fistula. Due to the similarity with other intestinal diseases, such as hemorrhoids, it is important to consult a doctor for an accurate diagnosis and appropriate treatment.
- Discharge of purulent-mucous masses: one of the main symptoms of rectal fistula is the discharge of purulent-mucous masses from the anus.
- Bleeding: the presence of bleeding after a bowel movement may be a sign of a rectal fistula.
- Pain in the anal area: pain occurring in the anal area, especially after defecation, may indicate a possible fistula.
- Itching and discomfort: accompanying pain may include itching and discomfort in the anal area with a rectal fistula.
- Discharge with an unpleasant odor: the presence of discharge from the anus with an unpleasant odor may be an additional symptom of a rectal fistula.
The specialists’ view on the methods of treating anal fistula
Expert opinions on the methods of treating rectal fistulas usually focus on an individualized approach for each patient. Conservative methods, such as antibiotics and applications, may be used in the early stages of the disease. However, in cases where conservative methods prove ineffective or the fistula becomes chronic, experts may suggest surgical intervention as a more radical treatment option, which often leads to the complete recovery of the patient.

Methods for diagnosing rectal fistula
For the diagnosis of rectal fistula, various methods are used, including rectal examination, which allows for the determination of the presence of discharge, tenderness, and other characteristics indicating a fistula. Endoscopy, such as colonoscopy, may be performed to visualize the internal structures of the intestines and identify pathologies, including fistulas. To clarify the diagnosis, CT or MRI studies may sometimes be required, which allow for a more detailed examination of the intestinal structure and reveal the possible presence of a fistula.
Effective diagnosis of rectal fistula plays an important role in determining treatment methods and planning surgical intervention. Alongside clinical signs, the implementation of various diagnostic procedures helps doctors establish an accurate diagnosis and choose the optimal treatment strategy for each patient considering the specifics of their condition.
- Rectal examination: The doctor performs a rectal examination to assess the presence of discharge, tenderness, or changes in the anal and rectal area.
- Colonoscopy: An endoscopic examination that allows visualization of the internal structures of the intestine and detection of pathologies, including fistulas.
- Computed tomography (CT): An imaging method that can be used for a more detailed study of the intestinal structure and identification of fistulas.
- Magnetic resonance imaging (MRI): An examination that provides detailed images of internal organs, including the rectum, to identify fistulas.
- Barium enema: A procedure in which a barium contrast agent is introduced into the rectum to detect abnormalities in the intestine, including fistulas.
Main methods of treating rectal fistula
- Surgical intervention: In the presence of a large or complicated rectal fistula, surgery may be required to remove the fistulous tract and restore normal bowel anatomy.
- Conservative treatment: In the case of a small fistula or absence of complications, conservative treatment may be applied, including the use of medications such as anti-inflammatory drugs or antibiotics.
- Planned observation: Regular monitoring of the patient’s condition and timely examinations help control the disease and prevent possible complications.
- Infusion therapy: In cases of acute infection or severe disease course, infusion therapy may be required to maintain fluid and electrolyte levels in the body.
- Physiotherapeutic procedures: During the rehabilitation period after surgery or as an additional treatment method, physiotherapeutic procedures may be used to improve tissue healing and alleviate symptoms.
Methods for preventing rectal fistula
- Healthy eating: A diet rich in fiber, fruits, vegetables, and regular water intake can promote gut health and reduce the risk of fistula formation.
- Physical activity: Regular moderate exercise can help maintain gut health and prevent inflammatory processes.
- Avoiding stress: Stress can negatively affect gut health, so stress management techniques can help in preventing rectal fistulas.
- Medical check-ups: Regular visits to the doctor, especially if there are risk factors, can help identify bowel pathologies at early stages and take preventive measures.
- Paying attention to gut flora: Maintaining a healthy gut microbiota through the consumption of prebiotics, probiotics, and synbiotics can contribute to gut health and prevent the development of fistulas.
Amazing aspects of rectal fistula
Moreover, a rectal fistula may sometimes need to be treated surgically, which underscores the importance of timely diagnosis and consulting a doctor when symptoms appear. Patients with this pathology need to receive appropriate medical care to prevent possible complications and preserve their quality of life.