Achilles tendonitis: diagnosis, risk factors, and treatment methods
- Definition and causes of Achilles tendonitis
- Factors contributing to the development of Achilles tendonitis
- The clinical picture of Achilles tendonitis
- Approaches to the treatment of Achilles tendonitis: expert opinions
- Methods for diagnosing Achilles tendonitis
- Principles of treating Achilles tendonitis
- Prevention measures for Achilles tendonitis
- Little-known facts about Achilles tendonitis
- FAQ
Definition and causes of Achilles tendonitis
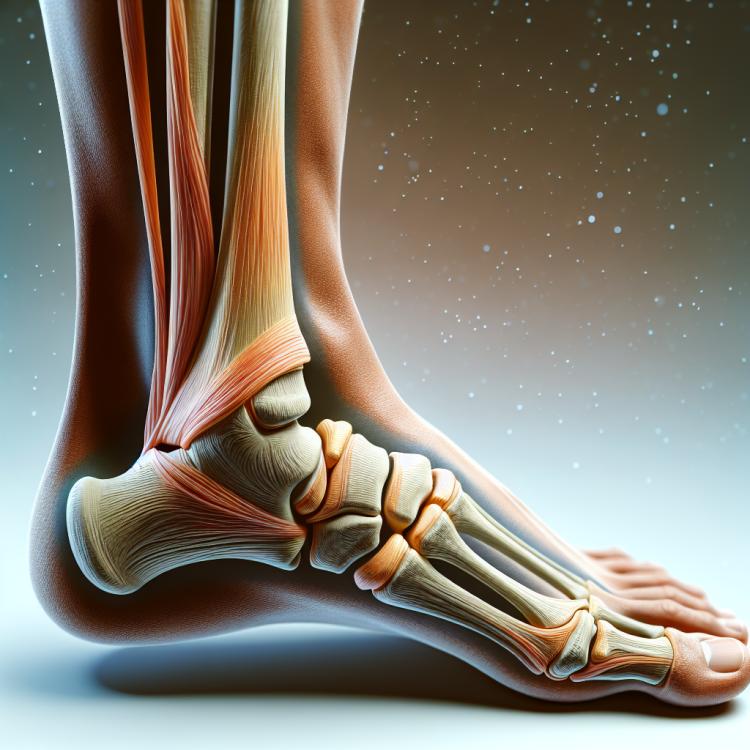
Achilles tendonitis is an inflammatory disease characterized by damage to the Achilles tendon, one of the largest and strongest tendons in the human body. The main cause of developing Achilles tendonitis is repetitive trauma and overload, leading to irritation and inflammation of the tendon.
Injuries can occur in athletes, especially with excessive loads on the muscles and tendons, as well as in people leading a sedentary lifestyle or suffering from obesity. The risk of developing Achilles tendonitis also increases with improper footwear or insufficient warm-up before physical exercises. It is important to seek medical help in a timely manner for diagnosis and comprehensive therapy of this disease.
Factors contributing to the development of Achilles tendonitis
Achilles tendonitis is an inflammatory condition that is most often caused by overload and trauma to the Achilles tendon. The main factors contributing to the development of Achilles tendonitis are increased load and frequent microtraumas to the area of the Achilles tendon, for example, during sports activities or due to improper footwear. The onset of the disease can also be influenced by disrupted biomechanics of the foot or an unbalanced training regimen, which leads to constant overload of the tendon and, ultimately, to the development of inflammation.
- Overload during physical activity: Intense training or participation in sports competitions can increase the risk of developing Achilles tendonitis.
- Failure to follow load recommendations: Inadequate distribution of load on the Achilles tendon during exercises can cause inflammation.
- Obesity: Excess weight increases the load on the Achilles tendon, contributing to its inflammation.
- Mechanical impact: Wearing uncomfortable or ill-fitting shoes can cause pressure and friction on the tendon.
- Foot and biomechanical anomalies: Mismatches in foot structure or walking biomechanics can create additional stress on the Achilles tendon, contributing to the development of tendonitis.
The clinical picture of Achilles tendonitis
Achilles tendonitis manifests with various symptoms, including pain and swelling in the area of the Achilles tendon, especially during physical activity or walking. Patients may also experience morning stiffness and pain when flexing the foot or jumping. Upon palpation near the Achilles tendon, thickening or swelling can be detected, as well as tenderness in this area.
In the case of Achilles tendonitis, a gradual worsening of symptoms over time is characteristic with prolonged use of the leg. Some patients report a decrease in overall foot mobility due to discomfort and pain. Diagnosis is based on the collection of medical history, clinical examination, and sometimes on additional tests, such as ultrasound or magnetic resonance imaging, to confirm the diagnosis.
- Pain in the area of the Achilles tendon: patients often experience pain during physical activity or when putting strain on the tendon.
- Swelling and thickening: swelling and thickening around the Achilles tendon may occur, especially upon palpation.
- tenderness when flexing the foot: pain may increase when flexing the foot or jumping, which is also a characteristic symptom.
- Morning stiffness: some patients notice stiffness and soreness in the area of the Achilles tendon after waking up in the morning.
- Decreased foot mobility: due to pain and discomfort, some patients may experience difficulty with normal foot movements.
Approaches to the treatment of Achilles tendonitis: expert opinions
Expert opinions on the treatment of achilles tendonitis highlight several key approaches. The initial phase of treatment usually involves the use of conservative methods, such as rest, therapeutic exercise, physical therapy, and wearing orthopedic shoes to reduce the load on the achilles tendon. Experts also emphasize the importance of early detection and diagnosis of the condition for successful treatment.
In cases where symptoms persist or the condition progresses, more intensive treatment methods may be employed, including corticosteroid injections, physical therapy, and surgical intervention in severe cases. Expert opinion also underscores that the treatment plan should be individualized, taking into account the specific characteristics of the patient and the nature of the injury, in order to achieve the best results and prevent recurrences.

Methods for diagnosing Achilles tendonitis
Diagnosis of Achilles tendonitis includes analysis of clinical symptoms, patient complaints, and medical history. Palpation and direct examination of the Achilles tendon can help identify thickening, swelling, or tenderness in the tendon area. To clarify the diagnosis and exclude other pathologies, instrumental methods such as ultrasound or magnetic resonance imaging are often used, which can help determine the extent of tissue damage.
Additional diagnostic methods, such as X-rays, may be useful to rule out fractures or other pathologies that can mimic the symptoms of tendonitis. Accurate and timely diagnosis plays an important role in determining the optimal treatment plan and preventing complications in Achilles tendonitis.
- Clinical examination: The doctor performs palpation and checks the area around the Achilles tendon for swelling, thickening, and tenderness.
- Ultrasound examination: A non-invasive method that allows visualizing tissues and assessing the structure and condition of the Achilles tendon.
- Magnetic resonance imaging (MRI): Provides a more detailed image of the tendon, detects injuries, and assesses the degree of inflammation.
- X-ray: Although it does not identify the tendinitis itself, it can be used to check the condition of the bones and rule out other pathologies, such as fractures.
- Clinical blood tests: A blood test may be performed to assess the level of inflammation and exclude other systemic diseases that may affect the condition of the tendon.
Principles of treating Achilles tendonitis
In cases where conservative methods do not provide the expected improvement, surgical intervention may be necessary. Surgical treatment of tendonitis can involve the removal of damaged tissue and rehabilitation of the Achilles tendon. A key aspect of successful treatment of Achilles tendonitis is an individualized approach that takes into account the characteristics of each patient and the severity of the condition.
- Rest and load limitation: the cornerstone of treating Achilles tendonitis is providing rest to the tendon to reduce inflammation and prevent further injury.
- Application of ice compresses: cold compresses can help reduce swelling and inflammation in the area of the Achilles tendon, aiding in pain relief and discomfort.
- Use of anti-inflammatory medications: a doctor may prescribe anti-inflammatory drugs to reduce inflammation and pain in the tendon area.
- Physical therapy: ultrasound therapy, laser treatment, and exercises for strengthening muscles and stretching can be effective methods in treating Achilles tendonitis.
- Surgical intervention: in cases where conservative methods do not lead to improvement, surgery may be necessary to remove damaged tissue and repair the Achilles tendon.
Prevention measures for Achilles tendonitis
Regular exercises to strengthen muscles and tendons, proper technique in performing sports movements, and following recommendations for moderation in loads will also help prevent injuries and the development of inflammatory processes in the area of the Achilles tendon. It is also important to monitor your overall health, including proper nutrition, hydration levels, and regular medical check-ups to timely identify and correct factors that may contribute to the onset of tendonitis.
- Adhering to appropriate loads: avoiding excessive loads and ensuring adequate time for recovery after workouts.
- Warm-up and stretching: performing a warm-up before physical exercises and regular stretching of tendons can help prevent injuries.
- Footwear control: choosing the right footwear for sports considering foot structure and limiting factors can reduce the risk of developing tendinitis.
- Strengthening muscles and tendons: regular exercises to strengthen the muscles of the ankle joint and tendons can help prevent possible overloads.
- Proper technique for exercises: learning the correct technique for performing sports movements and avoiding technical errors can reduce the risk of injuries.
Little-known facts about Achilles tendonitis
An interesting fact is that regular stretching and exercises to strengthen muscles and tendons can help prevent Achilles tendonitis. Adhering to the correct technique when performing exercises, choosing the right footwear, and taking individual characteristics into account while engaging in sports are also important for the prevention of this condition.