Trichomoniasis: diagnosis, prevention and consequences
- Definition of Trichomoniasis
- Etiology of Trichomoniasis
- Clinical picture of Trichomoniasis
- Experts’ opinions on the treatment of Trichomoniasis
- Methods for diagnosing Trichomoniasis
- Approaches to the treatment of Trichomoniasis
- Prevention measures for Trichomoniasis
- Interesting aspects of Trichomoniasis
- FAQ
Definition of Trichomoniasis
Trichomoniasis (also known as venereal disease) is an infection caused by the single-celled parasite Trichomonas vaginalis. It is transmitted through sexual contact. It is characterized by inflammation of the genital organs and unpleasant symptoms such as itching, burning, and pain during urination.
The diagnosis of trichomoniasis is made based on microscopic examination of vaginal secretions. Although this disease usually does not pose a serious health threat, it requires timely treatment with antimicrobial medications to prevent the transmission of the infection and reduce the risk of complications.
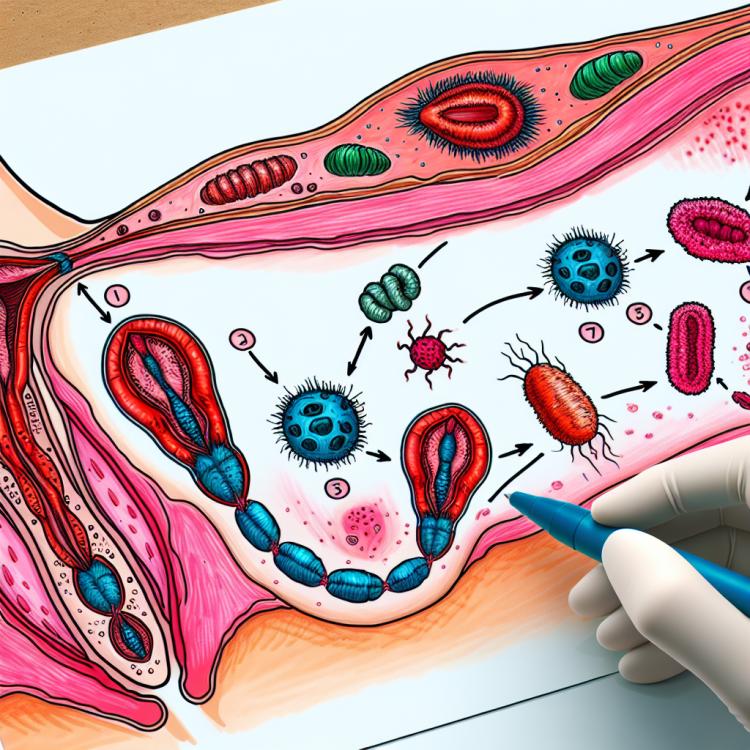
Etiology of Trichomoniasis
The etiology of trichomoniasis is due to the presence of the parasitic microorganism Trichomonas vaginalis, which is transmitted sexually. This microorganism is capable of colonizing the vagina and the human urethra, causing the corresponding infection.
The virulence factors of Trichomonas vaginalis include the adaptation to the mucous membrane and the ability to adhere to epithelial cells. These characteristics allow the parasite to survive and reproduce in the body, leading to the development of trichomoniasis in humans.
- Parasite Trichomonas vaginalis: the cause of trichomoniasis is the presence of the parasitic microorganism Trichomonas vaginalis, which is transmitted sexually.
- Sexual contact: transmission of Trichomonas vaginalis occurs during sexual relations without the use of condoms.
- Conditions of the vagina: a moist environment in the vagina can promote the reproduction and survival of Trichomonas vaginalis, contributing to the development of infection.
- Adaptation to epithelial cells: Trichomonas vaginalis has the ability to adapt to the cells of the mucous membrane, which facilitates its colonization.
- Adhesion to epithelial cells: the parasite’s ability to adhere to epithelial cells allows it to remain and multiply on the mucous membrane, causing infection.
Clinical picture of Trichomoniasis
The clinical picture of trichomoniasis may include vaginal itching, burning, discomfort, and pain during urination. Women often also experience changes in vaginal balance, vaginal discharge. In men, symptoms may manifest as itching in the urethral area, discomfort during urination, and possible discharge from the urethra.
Complications of trichomoniasis may include inflammatory processes in the genital area, which in turn can lead to more serious conditions such as cervicitis, urethritis, prostatitis, and other urinary tract infections.
- Vaginal itching: one of the most common symptoms of trichomoniasis is an unpleasant feeling of itching in the vagina.
- Burning and discomfort: patients often complain of burning sensations and discomfort in the genital area.
- Painful urination: trichomoniasis can cause painful sensations during urination in infected individuals.
- Changes in discharge: women often report changes in the consistency, color, and odor of vaginal discharge due to trichomoniasis infection.
- Symptoms in men: in men, trichomoniasis can manifest as itching, discharge from the urethra, and discomfort during urination.
Experts’ opinions on the treatment of Trichomoniasis
Experts in the field of infectious diseases usually recommend treating trichomoniasis with antiparasitic medications, including metronidazole or tinidazole. These medications are active against Trichomonas vaginalis and help eliminate the infection.
In addition, an important aspect of successful treatment is following the doctor’s recommendations, including taking medications as prescribed, ensuring stable treatment for the partner, and avoiding sexual contact during and until the treatment is completed. Supportive therapy and follow-up examinations can help prevent recurrences and additional complications.

Methods for diagnosing Trichomoniasis
Diagnosis of trichomoniasis may include clinical examination with medical history, microscopic examination of vaginal or urethral discharge for the presence of Trichomonas vaginalis, as well as laboratory tests such as PCR to confirm the infection. Cultural methods may also be used to cultivate and identify the pathogen.
Upon confirmation of the diagnosis, it is important to conduct comprehensive treatment, including the use of antiprotozoal drugs. After treatment, follow-up diagnostics are recommended to evaluate the effectiveness of therapy and to rule out disease recurrence.
- Clinical examination with history taking, identification of disease symptoms.
- Microscopic examination of vaginal or urethral discharge for the presence of Trichomonas vaginalis.
- Laboratory tests, including PCR to confirm parasitic infection.
- Cultivation and identification of the pathogen by cultural research methods.
- Follow-up diagnostics after treatment to assess therapy effectiveness and rule out disease recurrence.
Approaches to the treatment of Trichomoniasis
Given the possible side effects and contraindications, the course of treatment should be prescribed by a doctor, and the patient should follow the dosage instructions and duration of the medication. After completing the treatment, follow-up examinations are recommended to assess the success of the therapy and check for any recurrence of the infection.
- Treatment of trichomoniasis includes the use of antiprotozoal medications such as metronidazole or tinidazole to eliminate the parasites Trichomonas vaginalis.
- The optimal treatment regimen and dosage of medications are determined by the doctor based on the severity of the infection and the individual characteristics of the patient.
- Patients must strictly adhere to the recommendations for taking medications and the duration of the treatment course to achieve an effective result.
- After completing therapy, follow-up diagnostics are recommended to assess the effectiveness of the treatment and prevent possible recurrence of the infection.
- Patients should avoid sexual intercourse during treatment and ensure that their sexual partners also receive treatment to prevent reinfection.
Prevention measures for Trichomoniasis
Infected individuals’ partners are also advised to get tested and, if necessary, begin treatment to prevent reinfection. Education on sexual health, including information on protective methods, also plays an important role in the prevention of trichomoniasis.
- Avoid sexual contact with infected partners or use condoms to reduce the risk of transmission of infection.
- Regularly undergo medical examinations and screening tests for early detection and prevention of disease spread.
- Partners of infected individuals are recommended to get tested to prevent reinfection and local reinfection.
- Education and counseling on sexual health, including preventive measures, play a key role in preventing trichomoniasis.
- Maintaining personal hygiene and taking care of one’s own health also contribute to reducing the risk of infection and the spread of infection.
Interesting aspects of Trichomoniasis
It is also worth noting that Trichomonas vaginalis has a high mutation rate, which can create challenges in treating and controlling the infection. Studying these aspects helps develop more effective methods for diagnosing and treating trichomoniasis to combat this widespread disease.