Bacterial vaginosis: symptoms, causes, and treatment
- Interpretation of bacterial vaginosis
- Factors contributing to the development of bacterial vaginosis.
- Signs and symptoms of bacterial vaginosis
- Experts’ view on the treatment methods for bacterial vaginosis
- Methods for diagnosing bacterial vaginosis
- Modern methods of treating bacterial vaginosis
- Measures for the prevention of bacterial vaginosis
- Interesting aspects of bacterial vaginosis
- FAQ
Interpretation of bacterial vaginosis
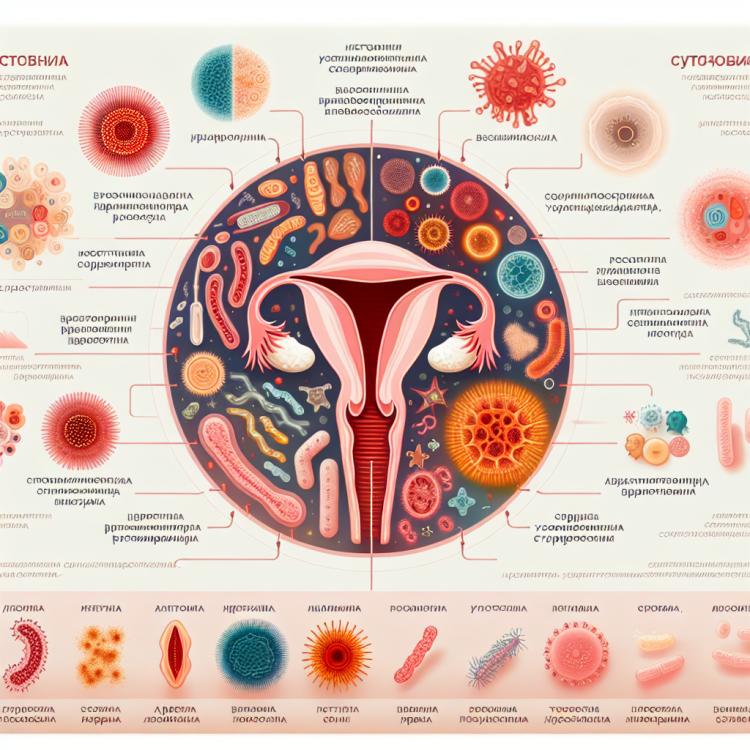
Bacterial vaginosis is a disorder of the vaginal microbiome characterized by an imbalance between beneficial and harmful microorganisms. The main cause of bacterial vaginosis is considered to be an increase in the number of bacteria of the genus Gardnerella vaginalis and a decrease in the number of lactobacilli, which leads to changes in the vaginal pH.
Characteristic symptoms of bacterial vaginosis include discharge with an unpleasant odor, watery or kefir-like consistency, as well as itching and irritation in the vaginal area. Diagnosis is based on the cellular composition of the discharge, vaginal pH, and the presence of characteristic bacteria. Treatment includes the use of antibiotics and probiotics to restore the natural balance of the microbiome.
Factors contributing to the development of bacterial vaginosis.
Bacterial vaginosis is caused by an imbalance of the vaginal microflora, leading to an increase in the number of bacteria such as Gardnerella vaginalis and a decrease in Lactobacillus, which play a key role in maintaining a healthy environment in the vagina. A number of factors are considered to contribute to the development of bacterial vaginosis, including decreased vaginal acidity, changes in estrogen levels, pregnancy, use of antibiotics, use of spermicides and douches for intimate hygiene, as well as sexual activity, especially with multiple partners.
- Decreased vaginal acidity: this creates a favorable environment for the reproduction of bacteria causing vaginosis.
- Changes in estrogen levels: for example, during menstruation or menopause, can contribute to changes in the vaginal microflora.
- Pregnancy: changes in hormonal background during pregnancy can also promote the development of bacterial vaginosis.
- Use of antibiotics: the use of antibiotics can disrupt the natural balance of microflora in the vagina, leading to the onset of bacterial vaginosis.
- Use of spermicides and douches for intimate hygiene: some chemicals in spermicides and douches can disrupt the vaginal flora, promoting the proliferation of pathogenic bacteria.
Signs and symptoms of bacterial vaginosis
Bacterial vaginosis can manifest with various symptoms, including changes in the moisture and odor of vaginal discharge. Usually, the secretions in bacterial vaginosis become watery and have a characteristic fishy smell that intensifies after sexual intercourse or between menstrual periods. However, in some women, bacterial vaginosis can be asymptomatic, making it difficult to diagnose the condition without laboratory analysis of the vaginal microflora.
- Change in the consistency of discharge: women with bacterial vaginosis may experience less thick and more liquid discharge, sometimes with a grayish-white tint.
- Odor of discharge: a characteristic fishy smell, especially intense after intercourse, is one of the main signs of bacterial vaginosis.
- Burning and itching in the vaginal area: some women may experience discomfort associated with a burning or itching sensation in the vagina.
- Discomfort during urination: bacterial vaginosis may be accompanied by discomfort or painful urination.
- Unusual sensations during sex: some women may experience unpleasant sensations or pain during intercourse when having bacterial vaginosis.
Experts’ view on the treatment methods for bacterial vaginosis
Experts in gynecology and infectious diseases are interested in the effectiveness of treating bacterial vaginosis with the involvement of probiotics and antibiotics. According to studies, probiotics such as Lactobacillus can help restore normal microflora in the vagina, which aids in combating imbalance and recurrences of the disease. However, in the presence of symptoms of bacterial vaginosis, consultation with a doctor is recommended to properly prescribe adequate treatment, including the use of antibiotics if necessary.

Methods for diagnosing bacterial vaginosis
The diagnosis of bacterial vaginosis usually involves a clinical examination taking into account the symptoms and the patient’s medical history. Additional diagnostic methods may include a vaginal examination and taking a swab from the vagina for laboratory analysis. When conducting laboratory studies, attention is paid to the vaginal pH level, microscopic examination of the swab for the presence of characteristic cells and bacteria, as well as culture studies to determine the type of microorganisms.
- Clinical examination: The doctor performs a visual and physical examination of the patient, identifying characteristic symptoms and signs of bacterial vaginosis.
- Vaginal examination: Allows for the assessment of the vaginal state for the presence of discharge, changes in microflora, and other pathologies.
- Microscopic examination of the smear: A laboratory procedure in which a specialist analyzes a smear with vaginal discharge under a microscope to identify characteristic cells and bacteria.
- Measurement of vaginal pH: A method aimed at assessing the acidity level of the vagina, as bacterial vaginosis is often accompanied by an increase in pH due to changes in microflora.
- Cultural examination of the smear: Allows for the growth and identification of the type of microorganisms present in the vagina for accurate diagnosis and selection of adequate therapy.
Modern methods of treating bacterial vaginosis
- Use of antibiotics: antibiotics such as metronidazole or clindamycin are often used to eliminate pathogenic bacteria causing bacterial vaginosis.
- Vaginal products: vaginal creams, gels, and suppositories containing metronidazole or other medications can be used for local action in the vagina.
- Probiotics: taking probiotics containing beneficial bacteria helps restore the balance of microflora in the vagina and prevent recurrences of the disease.
- Immune stimulation: strengthening the immune system with medications or methods that promote an increase in the body’s natural protective potential can help in the fight against bacterial vaginosis.
- Lifestyle changes: maintaining hygiene, refraining from using spermicides, and reducing stress can help in the prevention and treatment of bacterial vaginosis.
Measures for the prevention of bacterial vaginosis
- Hygiene of the genital organs: Daily gentle washing of the external genitalia with water, without the use of aggressive cleaning agents, helps maintain a healthy microflora in the vagina.
- Avoiding excessive use of antibacterial agents: Frequent use of soap or other antiseptics for intimate hygiene can disrupt the natural balance of microorganisms in the vagina, promoting the development of bacterial vaginosis.
- Choosing optimal contraception methods: When selecting contraceptives, it is important to discuss possible options and their impact on vaginal microflora with a doctor to avoid imbalance.
- Avoiding douching for intimate hygiene: Excessive use of douching for intimate hygiene can disrupt the natural pH of the vagina, creating conditions for the development of infections.
- Regular consultations with a gynecologist: Regular visits to the doctor can help identify possible changes in the condition of the vagina at an early stage and take necessary measures for disease prevention.