Vasculitis: Causes, Symptoms, and Treatment Methods
- Understanding vasculitis: symptoms, causes, and treatment.
- Factors contributing to the development of vasculitis
- Clinical manifestations of vasculitis
- Expert opinion on the treatment of vasculitis
- Methods for diagnosing vasculitis
- Methods of treating vasculitis
- Measures to prevent vasculitis
- Amazing aspects of vasculitis
- FAQ
Understanding vasculitis: symptoms, causes, and treatment.
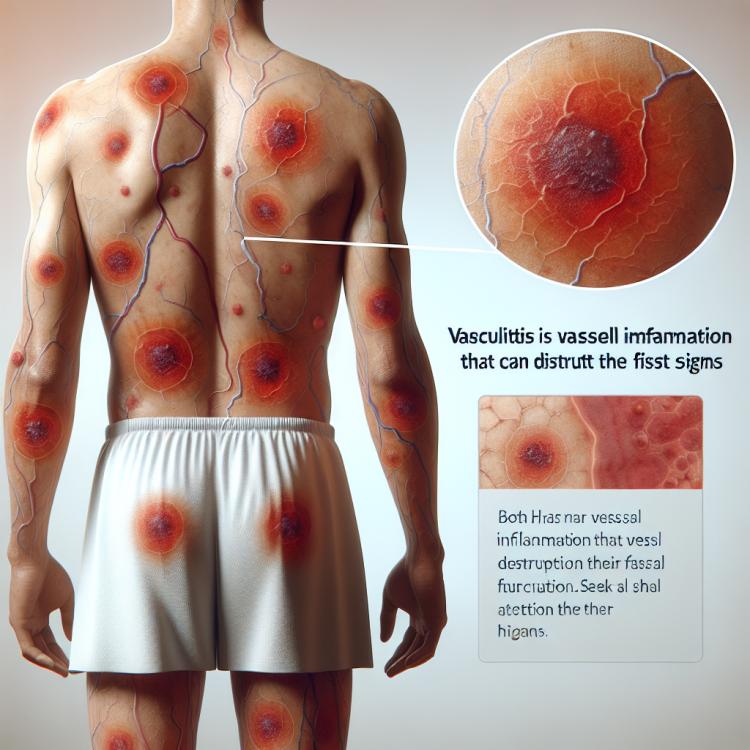
Vasculitis is an inflammatory disease of the blood vessels, which includes various types of inflammation of the vascular wall. Symptoms of vasculitis can vary depending on the type of the disease and include skin rashes, joint pain, elevated body temperature, and general weakness. Treatment of vasculitis typically involves the use of anti-inflammatory medications, immunosuppressants, as well as corticosteroids to control inflammation and reduce the risk of complications.
Factors contributing to the development of vasculitis
The development of vasculitis may be associated with various factors, including immunological disorders, infections, allergic reactions, and even some medications. Immune disorders often play a key role in the pathogenesis of vasculitis, causing inflammation and damage to the vascular wall. This can lead to impaired blood supply and organ damage, which is reflected in the diverse clinical manifestations of this disease.
- Immune disorders: Overactive immune systems can cause inflammation of the vessels, leading to the development of vasculitis.
- Infections: Some infectious agents can trigger the onset of vasculitis by provoking an immune response.
- Allergic reactions: Severe allergic reactions can cause inflammation of the vessels, contributing to the development of vasculitis.
- Medications: Some drugs can cause allergic or toxic reactions, leading to vasculitis in some cases.
- Genetic predisposition: Certain genetic factors can increase the risk of developing vasculitis, making some individuals more susceptible to this condition.
Clinical manifestations of vasculitis
The symptoms of vasculitis depend on the type of affected vessels and organs, but generally include skin changes, arthralgias, fever, fatigue, and weight loss. Patients with vasculitis often exhibit skin lesions such as petechiae, cyanosis, and Raynaud’s syndrome associated with peripheral vessels. Additionally, vasculitis can cause problems with organs such as the kidneys, heart, lungs, or nervous system, which further complicates the course of the disease.
- Rash and skin changes: include red spots, bruises, ulcers, or rashes typical of various forms of vasculitis.
- arthralgias: joint pain can be a symptom of vasculitis, especially when large joints are affected.
- Fever: an increase in body temperature to high values carries important information about the inflammatory process characteristic of vasculitis.
- Fatigue: a feeling of tiredness and general weakness may accompany vasculitis due to chronic inflammation and organ dysfunction.
- Weight loss: significant weight loss can be a sign of the inflammatory process characteristic of vasculitis.
Expert opinion on the treatment of vasculitis
The expert opinion on the treatment of vasculitis is based on a comprehensive approach that takes into account the type and severity of the disease, the patient’s comorbid conditions, and the potential side effects of the medications used. Experts recommend an individualized approach to treatment, including the use of immunotherapy, glucocorticosteroids, cytostatics, and other medications depending on the clinical picture.
Modern treatment methods for vasculitis aim not only to suppress inflammation but also to prevent relapses and reduce the risk of complications. Experts emphasize the importance of regular monitoring of the patient’s condition as well as educating patients to independently manage their disease and adhere to specialists’ recommendations.

Methods for diagnosing vasculitis
The diagnosis of vasculitis involves a combination of methods, starting with the examination and history of the patient, as well as laboratory and instrumental studies. Laboratory tests may include a complete blood count, biochemical studies, and immunological tests to identify specific antibodies and inflammation markers. Instrumental methods, such as angiography, biopsy of affected tissues, and educational diagnostics, may be used for a more accurate assessment of the condition of the blood vessels and organs, which helps to establish the correct diagnosis and determine the treatment strategy.
- Physical examination and history: The doctor may pay attention to characteristic symptoms of vasculitis and ask questions about possible causes of the disease.
- Laboratory blood tests: A complete blood count allows for the assessment of inflammatory markers, such as elevated levels of C-reactive protein or erythrocyte sedimentation rate.
- Immunological tests: Tests for specific antibodies, such as ANA (antinuclear antibodies) or ANCA (antineutrophil cytoplasmic antibodies), can help clarify the diagnosis of vasculitis.
- Instrumental methods: Angiography, biopsy of affected tissues, computed tomography, and X-rays can help visualize changes in the vessels and organs affected by vasculitis.
- Ultrasound examination: Ultrasound can be used to assess blood vessels and pathological changes in tissues, aiding in the diagnosis of vasculitis.
Methods of treating vasculitis
A personalized approach to the treatment of vasculitis should take into account the characteristics of each patient, their overall health status, possible complications, and the effectiveness of the medications used. Comprehensive treatment includes not only pharmacotherapy but also rehabilitation activities, supportive therapy, as well as regular medical monitoring to control the disease state and prevent possible complications.
- Anti-inflammatory drugs: The use of glucocorticoids and non-steroidal anti-inflammatory medications to reduce inflammation and symptoms.
- Immunosuppressants: The use of medications that reduce the activity of the immune system to suppress the autoimmune response.
- Immunomodulators: Drugs aimed at regulating the immune system can be used to stabilize the disease.
- Biological therapy: The use of biological products that act on specific molecular targets to improve control over vasculitis.
- Rehabilitation activities: Physiotherapy, psychotherapy, and a balanced diet can be important components of comprehensive vasculitis treatment.
Measures to prevent vasculitis
Adhering to a healthy lifestyle, including a balanced diet, physical exercise, quitting smoking, and moderate alcohol consumption, also contributes to the prevention of vasculitis. Regular medical check-ups, especially in the presence of risk factors, help to detect early signs of the disease and initiate treatment in the early stages, which facilitates more effective disease management.
- Disease and condition control: regular examinations to identify and monitor the main causes that contribute to the development of vasculitis.
- Healthy lifestyle: maintaining a healthy lifestyle, including a balanced diet, physical activity, and avoiding harmful habits (smoking, alcohol consumption).
- Regular medical consultations: visiting a doctor to monitor health and identify early signs of vasculitis.
- Follow doctor’s recommendations: adhering to individual recommendations from a specialist for disease prevention and monitoring.
- Avoiding risk factors: preventing contact with known triggers of vasculitis, such as infections or medications that may provoke the development of the disease.
Amazing aspects of vasculitis
Understanding the mechanisms of vasculitis development remains a subject of active research in medical science. Studies in this area expand our knowledge of the pathogenesis of the disease, opening new perspectives for improving the diagnosis, treatment, and prevention of vasculitis.